Candidiasis is a fungal infection caused by yeasts from the genus Candida. Candida albicans is the predominant cause of the disease.
Signs and symptoms
Chronic mucocutaneous candidiasis
Findings reveal disfiguring lesions of the face, scalp, hands, and nails. Chronic mucocutaneous candidiasis occasionally is associated with oral thrush and vitiligo.
Oropharyngeal candidiasis
Individuals with oropharyngeal candidiasis (OPC) usually have a history of HIV infection, wear dentures, have diabetes mellitus, or have been exposed to broad-spectrum allopathic antibiotics or inhaled steroids. Although patients frequently are asymptomatic, when symptoms do occur, they can include the following:
- Sore and painful mouth,
- Burning mouth or tongue,
- Dysphagia,
- Thick, whitish patches on the oral mucosa.
Physical examination reveals a diffuse erythema and white patches that appear on the surfaces of the buccal mucosa, throat, tongue, and gums.
Types of oropharyngeal candidiasis
The following are the 5 types of oropharyngeal candidiasis:
- Membranous candidiasis – One of the most common types; characterized by creamy-white, curdlike patches on the mucosal surfaces,
- Chronic atrophic candidiasis (denture stomatitis) – Also thought to be one of the most common forms of the disease; presenting signs and symptoms include chronic erythema and edema of the portion of the palate that comes into contact with dentures,
- Erythematous candidiasis – Associated with an erythematous patch on the hard and soft palates.
- Angular cheilitis – Inflammatory reaction characterized by soreness, erythema, and fissuring at the corners of the mouth,
- Mixed – A combination of any of the above types is possible.
Esophageal candidiasis
Patients with esophageal candidiasis may be asymptomatic or may have 1 or more of the following symptoms: 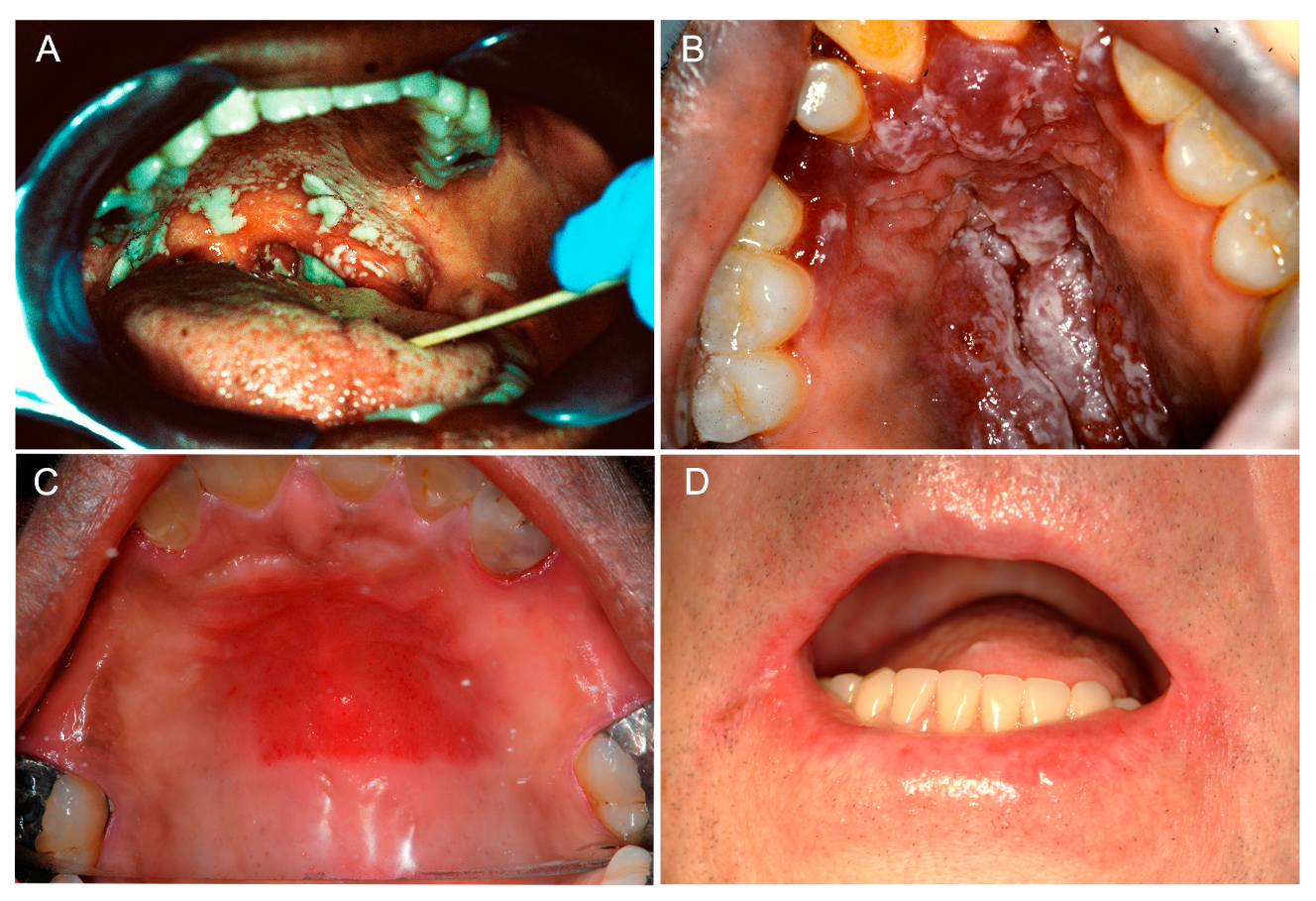
- Normal oral mucosa (>50% of patients).
- Dysphagia.
- Odynophagia.
- Retrosternal pain.
- Epigastric pain.
- Nausea and vomiting.
Physical examination almost always reveals oral candidiasis.
Nonesophageal gastrointestinal candidiasis
The following symptoms may be present:
- Epigastric pain.
- Nausea and vomiting.
- Abdominal pain.
- Fever and chills.
- Abdominal mass (in some cases).
Genitourinary tract candidiasis
The types of genitourinary tract candidiasis are as follows:
- Vulvovaginal candidiasis (VVC) – Erythematous vagina and labia; a thick, curd like discharge; and a normal cervix upon speculum examination.
- Candida balanitis – Penile pruritus and whitish patches on the penis.
- Candida cystitis – Many patients are asymptomatic, but bladder invasion may result in frequency, urgency, dysuria, hematuria, and suprapubic pain.
- Asymptomatic candiduria – Most catheterized patients with persistent candiduria are asymptomatic.
- Ascending pyelonephritis – Flank pain, abdominal cramps, nausea, vomiting, fever, chills and hematuria.
- Fungal balls – Intermittent urinary tract obstruction with subsequent anuria and ensuing renal insufficiency.
Diagnosis
Diagnostic tests for candidiasis include the following:
- Mucocutaneous candidiasis – For a wet mount, scrapings or smears obtained from skin, nails, or oral or vaginal mucosa are examined under the microscope; a potassium hydroxide smear, Gram stain, or methylene blue is useful for direct demonstration of fungal cells.
- Cutaneous candidiasis – Using a wet mount, scrapings or smears obtained from skin or nails can be examined under the microscope; potassium hydroxide smears are also useful.
- Genitourinary candidiasis – A urinalysis should be performed; evidence of white blood cells (WBCs), red blood cells (RBCs), protein, and yeast cells is common; urine fungal cultures are useful.
- Gastrointestinal candidiasis – Endoscopy with or without biopsy.

Lab results
Unfortunately, results from the routine laboratory studies are often nonspecific and not very helpful. Clinicians are required to act definitively and early based on a high index of suspicion. In the past, many patients with life-threatening candidiasis died without receiving antifungal therapy.
Systemic candidiasis should be suspected in patients with persistent leukocytosis and either persistent neutropenia or other risk factors and who remain febrile despite broad-spectrum antibiotic therapy. To be effective, antifungal therapy should be provided early and empirically in such high-risk patients. Cultures of nonsterile sites, although not useful for establishing a diagnosis, may demonstrate high degrees of candidal colonization. Always consider positive culture results from sterile sites to be significant and evidence of infection.
Allopathic treatment for candidiasis
Cutaneous candidiasis
Most localized cutaneous candidiasis infections may be treated with any number of topical antifungal agents (eg, clotrimazole, econazole, ciclopirox, miconazole, ketoconazole, nystatin). If the infection is a paronychia, the most important aspect of therapy is drainage of the abscess, followed by oral antifungal therapy with either fluconazole or itraconazole. In cases of extensive cutaneous infections, infections in immunocompromised patients, folliculitis, or onychomycosis, systemic antifungal therapy is recommended. For Candida onychomycosis, oral itraconazole (Sporanox) appears to be most efficacious. Two treatment regimens are available: the daily dose of itraconazole taken for 3-6 months or the pulsed-dose regimen that requires a slightly higher daily dose for 7 days, followed by 3 weeks of no drug administration. The cycle is repeated every month for 3-6 months.
Gastrointestinal candidiasis
Oropharyngeal candidiasis
Oropharyngeal candidiasis OPC can be treated with either topical antifungal agents (eg, nystatin, clotrimazole, amphotericin B oral suspension) or systemic oral azoles (fluconazole, itraconazole, or posaconazole).
Infections in HIV-positive patients tend to respond more slowly and, in approximately 60% of patients, recur within 6 months of the initial episode. Approximately 3-5% of patients with advanced HIV infection (CD4 cell counts < 50/µL) may develop refractory OPC. In these situations, in addition to attempting correction of the immune dysfunction with HAART, higher doses of fluconazole (up to 800 mg/d) or itraconazole (up to 600 mg/d) can be attempted. Posaconazole suspension at 400 mg orally twice per day has also yielded excellent results in such patients. Additionally, caspofungin 50 mg/d IV and anidulafungin 100 mg/d IV have also yielded excellent efficacy in such patents. Amphotericin B is rarely necessary to treat such cases, but, when used, low doses of amphotericin B can be used (0.3-0.7 mg/kg) and have been shown to be effective. 
Candida esophagitis
Esophageal candidiasis should always be treated with systemic agents and not topical agents. The most commonly used medication to treat esophageal candidiasis is oral fluconazole 200 to 400 mg per day for 14 to 21 days. If patients cannot tolerate oral intake, then intravenous Fluconazole 400 mg daily can be used and then de-escalated to oral Fluconazole when the patient can tolerate oral medications. Fluconazole 100 to 200 mg three times per week can be used to suppress recurrent esophageal candidiasis.
Micafungin 150 mg IV daily has been shown to be non-inferior to fluconazole at 200 mg daily. Itraconazole 200 mg per day orally or Voriconazole 200 mg twice daily for 14 to 21 days are other treatment options. Amphotericin B deoxycholate 0.3 to 0.7 mg/kg daily can be used in patients with refractory candida esophagitis, but it has serious medication side effects and should be avoided if possible. Posaconazole 400 mg twice daily has been effective in refractory esophageal candidiasis as well.
One may also use caspofungin as it is preferred over amphotericin.
The dose of the azole agents does need modification in patients with renal insufficiency. Azoles are considered teratogenic, so in pregnant patients with esophageal candidiasis, Amphotericin B is preferred.
Genitourinary tract candidiasis
Vulvovaginal candidiasis (VVC) can be managed with either topical antifungal agents or a single dose of oral fluconazole. A single dose of oral fluconazole (150 mg) in acute episodes of VVC has been shown to yield clinical and microbiological efficacy as good as or better than topical antifungal agents. A small percentage (< 5%) of women experience chronic recurrent VVC infections, which often require long-term or prophylactic oral azole therapy for control. In such patients, the recommended regimen includes fluconazole 150 mg every other day for 3 doses, followed by weekly fluconazole 150-200 mg for 6 months.
This regimen prevents further recurrence in more than 80% of women. In pregnant women, just one or two oral doses of fluconazole for vaginal candidiasis during pregnancy was not associated with significantly increased risks of stillbirth or neonatal death, according to a 2018 Scandinavian cohort study.
Ibrexafungerp (Brexafemme)
The first and only allopathic treatment for vaginal yeast infections which is both oral and a non-azole, has been approved for the treatment of VVC. Its mechanism of action is glucan synthase inhibition with broad-spectrum anti-Candida fungicidal activity. 
Oteseconazole
A tetrazole, oral, antifungal has recently been approved for recurrent VVC, becoming the first drug approved for this indication. Recommended regimen consists of 11 weekly doses two weeks after an initial 2-day loading dose course.
For asymptomatic candiduria, therapy generally depends on the presence or absence of an indwelling Foley catheter. Candiduria frequently resolves by simply changing the Foley catheter (20-25% of patients).
Allopathic experts thinks that asymptomatic candiduria associated with a Foley catheter does not require treatment in most cases. However, eradicating candiduria prior to any form of instrumentation or urological manipulation is prudent.
Candida cystitis in noncatheterized patients should be treated with fluconazole at 200 mg/d orally for at least 10-14 days. For Candida cystitis in catheterized patients, the first step is always to remove the nidus of infection. Thus, the Foley catheter should be removed or replaced prior to initiating antifungal therapy. If the candiduria persists after the catheter change, then patients can be treated with 200 mg/d of fluconazole orally for 14 days. Alternative therapy includes amphotericin B bladder irrigation.
Urinary catheter
However, its use for the treatment of funguria is significantly limited, primarily because of the required maintenance of a urinary catheter; lack of adequate studies to define the dose, duration, and method of administration; restriction of its use to uncomplicated lower urinary tract infections; and the availability of more convenient treatment options (eg, oral fluconazole therapy). The use of amphotericin B bladder irrigation is rarely needed.
Administering intravenous amphotericin B to treat candiduria is rarely necessary.
Renal candidiasis
Regardless of whether the infection involves hematogenous dissemination to the kidney or ascending infection (pyelonephritis), systemic antifungal therapy is required. The most recent comparative studies indicate that fluconazole at 400 mg/d intravenously or orally for a minimum of 2 weeks is as effective as amphotericin B without the toxicities normally associated with amphotericin B. For amphotericin B, the daily dose is 0.5-0.7 mg/kg intravenously for a total dose of 1-2 g administered over a 4- to 6-week period.
Candidemia
This requires treatment in all patient populations. Current recommendations depend on the presence or absence of neutropenia. 
In patients without neutropenia, an echinocandin is recommended as initial therapy and fluconazole an acceptable alternative in certain circumstamces in most cases of candidemia and disseminated candidiasis. Transition to fluconazole is also possible when clinically stable and a fluconazole-susceptible strain is identified. Studies conducted by the MSG have demonstrated that fluconazole at a dose of 400 mg/d is as efficacious as amphotericin B.
Thus, once the gastrointestinal tract is functional, the parenteral antifungal may be switched to the oral formulation with the same efficacy. Alternative options listed below need to be considered depending on history of previous exposure to antifungals, the probability of fluconazole resistance according to the species of Candida recovered, the presence of comorbid conditions, and the clinical status of the patient.
An echinocandin is recommended for candidemia in most patients with neutropenia. Lipid amphotericin B is an alternative that can be considered. Fluconazole is an alternative in patients who are less critically ill and who have no recent azole exposure. Voriconazole can be used when additional mold coverage is desired.
Dosage for fluconazole
The standard recommended dose for fluconazole is 800 mg as the loading dose, followed by fluconazole at a dose of 400 mg/d for at least 2 weeks of therapy after a demonstrated negative blood culture result or clinical signs of improvement. This treatment regimen can be used for infections due to C albicans, C tropicalis, C parapsilosis, C kefyr, C dubliniensis, C lusitaniae, and C guilliermondi.
A critical component in the management of candidemia and disseminated candidiasis is the removal of the focus of infection, such as intravenous and Foley catheters.
Echinocandins
Available echinocandins for candidemia include the following:
Caspofungin (Cancidas)
It can be initiated as a 70-mg loading dose, followed by 50 mg/d intravenously to complete a minimum of 2 weeks of antifungals after improvement and after blood cultures have cleared. Caspofungin is a broad-spectrum semisynthetic echinocandin. It is an effective alternative for severe mucosal infections and systemic infections due to Candida, especially those due to non-albicans Candida species such as C glabrata.
Anidulafungin
It can be initiated as a 200-mg loading dose, followed by 100 mg intravenously to complete a minimum of 2 weeks of antifungals after improvement and after blood cultures have cleared. Anidulafungin is a broad-spectrum echinocandin. It is an effective alternative for severe mucosal infections and systemic infections due to Candida, especially those due to non-albicans Candida species such as C glabrata. 
Micafungin
It can be administered at 100 mg/d intravenously to complete a minimum of 2 weeks of antifungals after improvement and after blood cultures have cleared. Micafungin is a broad-spectrum echinocandin. It has been shown to be an effective alternative for severe mucosal infections and systemic infections due to Candida, especially those due to non-albicans Candida species such as C glabrata.
Rezafungin
Also call Rezzayo is initiated with a 400-mg IV loading dose, then 200 mg intravenously once weekly for up to 4 doses. It is indicated for adults who have limited or no alternative treatment options for candidemia and invasive candidiasis, as shown in clinical trials. Rezafungin has shown antifungal activity against C albicans, C glabrata, C parapsilosis, and C tropicalis. It also is under investigation for prevention of candidiasis in bone marrow transplant. Weekly administration offers the potential to ambulatory management of difficult to treat candidiasis.
Additional options
Additional options for candidemia include the following:
- Voriconazole can be initiated at 6 mg/kg intravenously or orally twice per day, followed by 3 mg/kg orally twice per day or 200 mg orally twice per day. Based on the findings from a global multicenter clinical trial, voriconazole has also been approved for use in candidemia in patients who are not neutropenic.
- Amphotericin B deoxycholate can be administered at 0.7 mg/kg/d intravenously for a total dose of 1-2 g over a 4- to 6-week period.
- Liposomal preparations of amphotericin B have comparable efficacy to conventional amphotericin B, but renal toxicity is considerably less common with the former.
Chronic mucocutaneous candidiasis
This condition is generally treated with oral azoles, such as fluconazole at a dose of 100-400 mg/d or itraconazole at a dose of 200-600 mg/d until the patient improves. The initial therapy for acute infection is always followed by maintenance therapy with the same azole for life.
Hepatosplenic candidiasis
Induction therapy is initially started with amphotericin B deoxycholate for at least 2 weeks, followed by consolidation therapy with fluconazole at a dose of 400 mg/d for an additional 4-12 weeks depending on the response. 
Respiratory tract candidiasis
If the diagnosis is established based on biopsy findings, then the infection is treated as disseminated candidiasis.
Invasive candidiasis
Empirical treatment options for suspected invasive candidiasis include the following:
- Empirical antifungal therapy should be considered for critically ill patients with risk factors for invasive candidiasis and no other cause of fever, and it should be based on clinical assessment of risk factors, serologic markers for invasive candidiasis, and/or culture data from nonsterile sites. (Its benefits have not been clearly determined.).
- This continues to be a problematic decision since criteria for starting empirical antifungal therapy remain poorly defined. Empirical therapy in persistently febrile and neutropenic patients should cover infections caused by yeasts and molds.
- The choice of drugs in nonneutropenic patients is similar to that for proven candidiasis. Recommended agents include fluconazole or an echinocandin.
- In neutropenic patients, a lipid formulation of amphotericin B, caspofungin, or voriconazole is recommended. Azoles should not be used for empirical therapy in individuals who have received an azole for prophylaxis.
Disseminated candidiasis with end organ infection
Disseminated candidiasis with end organ involvement requires an individualized approach. Thus, the manifestation of invasive candidiasis involving localized structures, such as in Candida osteomyelitis, arthritis, endocarditis, pericarditis, and meningitis, requires prolonged antifungal therapy for at least 4-6 weeks.
Fluconazole
The optimum dosage and duration of therapy for various types of deep candidal infection have not been definitively determined. The standard recommended dose for most Candida infections is fluconazole at 800 mg as the loading dose, followed by fluconazole at a dose of 400 mg/d either intravenously or orally for at least 2 weeks of therapy after a demonstrated negative blood culture result or clinical signs of improvement.
Caspofungin (Cancidas)
It can be initiated as a 70-mg loading dose, followed by 50 mg/d intravenously to complete a minimum of 2 weeks of antifungals after improvement and after blood cultures have cleared. Caspofungin is a broad-spectrum semisynthetic echinocandin. It is an effective alternative for severe mucosal infections and systemic infections due to Candida, especially those due to non-albicans Candida species such as C glabrata. 
Anidulafungin
This drug can be initiated as a 200-mg loading dose, followed by 100 mg intravenously to complete a minimum of 2 weeks of antifungals after improvement and after blood cultures have cleared. Anidulafungin is a broad-spectrum echinocandin. It is an effective alternative for severe mucosal infections and systemic infections due to Candida, especially those due to non-albicans Candida species such as C glabrata.
Micafungin
It can be administered at 100 mg/d intravenously to complete a minimum of 2 weeks of antifungals after improvement and after blood cultures have cleared. [67, 68] Micafungin is a broad-spectrum echinocandin. It has been shown to be an effective alternative for severe mucosal infections and systemic infections due to Candida, especially those due to non-albicans Candida species such as C glabrata.
Voriconazol
It can be initiated at 6 mg/kg intravenously or orally twice per day, followed by 3 mg/kg orally twice per day or 200 mg orally twice per day. Based on the findings from a global multicenter clinical trial, voriconazole has also been approved for use in candidemia in patients who are not neutropenic.
Rezafungin (Rezzayo)
Is initiated with a 400-mg IV loading dose, then 200 mg IV once weekly for up to 4 doses. It is indicated for adults who have limited or no alternative treatment options for candidemia and invasive candidiasis. Shown to have antifungal activity against C albicans, C glabrata, C parapsilosis, and C tropicalis.
Amphotericin B deoxycholate
It has been an alternative to fluconazole for many years. However, with the advent of the newer azoles and the echinocandins, its role as a primary or secondary option needs to be reconsidered. The dose for amphotericin B deoxycholate is 0.5-0.7 mg/kg/d intravenously to achieve a minimum of 1- to 2-g total dose.
For the treatment of invasive candidiasis caused by less-susceptible species, such as C glabrata and C krusei, higher doses (up to 1 mg/kg/d) should be considered.
Liposomal preparations of amphotericin B are recommended at doses between 3 and 5 mg/kg/d when used for invasive candidiasis.
Special situations involving antifungal resistance
Several of the Candida species require special mention because of their known intrinsic resistance to antifungals. 
Because C glabrata is known to be resistant to fluconazole in 15-25% of cases and has decreased susceptibility to most antifungals, C glabrata infections require a change in conventional antifungal therapy. The drugs of choice for such infections are the echinocandins: caspofungin 70 mg intravenously as a loading dose, followed by 50 mg/d; anidulafungin 200-mg loading dose, followed by 100 mg/d; or micafungin 100 mg/day intravenously. An alternative is voriconazole at 6 mg/kg administered twice on the first day, followed by 3 mg/kg twice per day or 200 mg twice per day orally; other options include amphotericin B deoxycholate (1 mg/kg/d), or lipid preparations of amphotericin B at 3-5 mg/kg/d.
If in vitro susceptibility assays are available, it may be worthwhile to establish the in vitro susceptibility of the C glabrata strain to fluconazole. If the MIC is less than 8 μg/mL, then fluconazole can be used at 400 mg/d intravenously or orally.
C krusei infections
They necessitate the use of an agent other than fluconazole, because this organism is intrinsically resistant to fluconazole and has a decreased susceptibility to itraconazole, ketoconazole, and amphotericin B. Thus, the preferred regimen includes echinocandins (caspofungin, anidulafungin, or micafungin) voriconazole, or amphotericin B at 1 mg/kg/d. Infections due to C lusitaniae or C guilliermondi necessitate the use of fluconazole, voriconazole, or the echinocandins because these isolates are frequently intrinsically resistant to amphotericin B or develop resistance to amphotericin B while the patient is on therapy.
New drugs
Newer agents with recent approval or already in clinical trials include:
- rezafungin, a long-acting echinocandin given weekly and indicated for candidemia and invasive candidiasis,
- ibrexafungerp, a glucan-synthase inhibitor, that was approved in 2021 for the treatment of vulvo-vaginal candidiasis in oral formulation. The parenteral formulation is still under investigation for the treatment of candidemia and invasive candidiasis.
- fosmanogepix, prodrug of manogepix, with a novel mechanism of action (inhibition of Gwt1 enzyme that affects the anchoring of mannoproteins to the fungal cell wall, impairing adherence to mucosal and epithelial surfaces, compromising the cell wall integrity, and affecting biofilm formation).
Surgical Care
Major organ infections associated with candidal abscess formation may require surgical drainage procedures along with the appropriate antifungal therapy. Prosthetic joint infection with Candida species requires the removal of the prosthesis. Surgical debridement is generally necessary for sternal infections and frequently for vertebral osteomyelitis. 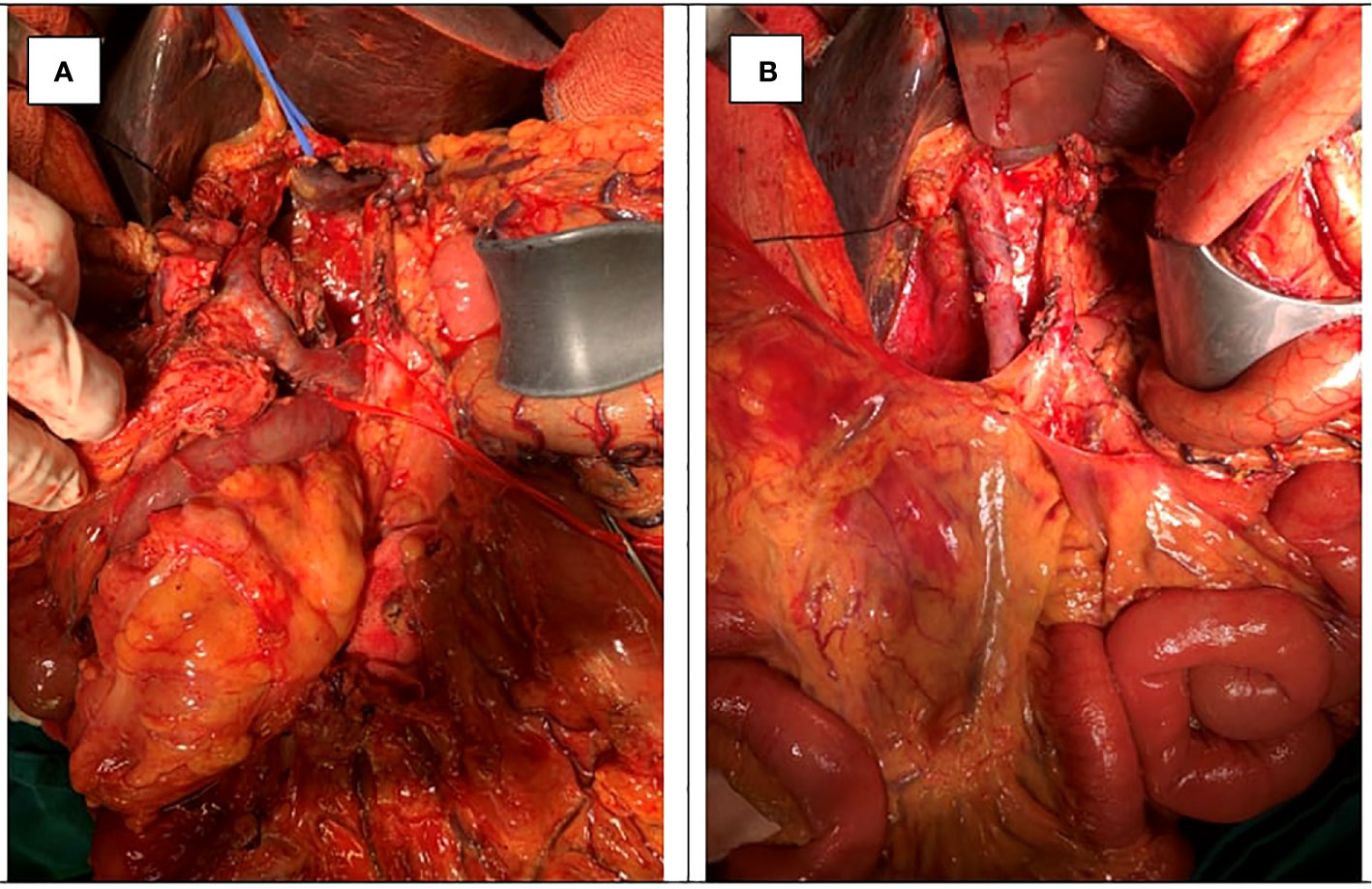
Splenic abscesses occasionally require splenectomy.
Valve replacement surgery needs to be considered to treat endocarditis. Most reviews have favored consideration for surgery.
In addition to medical management, vitrectomy is a therapeutic option in fungal endophthalmitis.
Side Effects of allopathic drugs
In August 2013, the WHO announced that clinicians should no longer prescribe ketoconazole (Nizoral, Janssen Pharmaceuticals) tablets as a first-line therapy for any fungal infection, including Candida and dermatophyte infections, because of the risk for severe liver injury, adrenal insufficiency, and adverse drug interactions.
Homeopathic treatment / Management for candidiasis
Homeopathy or “similar therapy” is a phylum of “alternative medicines” is belonging to 7000 years ago. Hippocrates (350 -460 BC) had used homeopathic remedies to cure his patients, and he believed, we should cure similar with similar (Salehi, 2011). Jalinus (130 -200AC) was a famous anatomist, physiologist and homeopath. His books were used to cure the patients during about 1000 years. Samuel Hahnemann was a German physician and chemist; he proved some of the homeopathic remedies on him and established the symptoms in the books: “organon of medicines” is about the philosophy of homeopathy and “rules of homeopathy” (1805), “chronic diseases” and “Materia medica pura”.
In Homeopathy, there are dozens of well proven medicines for candidiasis doctors are prescribing from centuries. They have no known side effects and are permanent treatment for any viral and bacterial infections. Here are few of them:
Sepia Succus
Sepia Succus is a medicine for yeast infections like candidiasis, ringworm (skin) {tinea corporis}, leucorrhea and vaginal candidiasis. Boils and blood-boils. Engorged glands (Bartholin Gland). Eruptions of vesicles, like pemphigus. Sexual organs cold. Offensive perspiration. Gleet; discharge from urethra only during night; no pain. Condylomata surround head of penis. Violent stitches upward in the vagina.
Ringworm and yeast infection in men and women. Tongue white. Taste salty, putrid. Tongue foul but clears during menses. Swelling and cracking of lower lip. Pain in teeth from 6pm till midnight; worse on lying. Thick, greenish nasal discharge; thick plugs and crusts. Yellowish saddle across nose.
Herpes circinatus in isolated spots. Itching; not relieved by scratching; worse in bends of elbows and knees. Chloasma; herpetic eruption on lips, about mouth and nose. Ringworm-like eruption every spring. Urticaria on going in open air; better in warm room. Sweat of intolerable odor. Lentigo in women. Ichthyosis with offensive odor of skin.
Tongue white. Taste salty, putrid. Swelling and cracking of lower lip. Dyspepsia. Everything tastes too salty. Nausea in morning before eating. Disposition to vomit after eating. Burning in pit of stomach. Flatulent, with headache. Liver sore and painful. Many brown spots on abdomen. Feeling of relaxation and bearing down in abdomen. Prolapsus ani. Almost constant oozing from anus.
Silicea Terra or Silica
Yeast infection (condidiasis) in men and women especially in groins. Discharge of blood before proper period; menses too late; protracted; blood acrid. Metrorrhagia. Diarrhea, before the menses. Painful menses, pale appearance of objects, or burning sensation and excoriation in vulva.
Itching in the vulva. Pressing down feeling in vagina. Itching, burning, and soreness in pudenda. Leucorrhea, which flows when urinating, or after the menses. Leucorrhea, like milk, flowing at intervals, and preceded by griping in umbilical region. Acrid, corrosive leucorrhea. Leucorrhea and vaginal candidiasis.
Fetid otorrhea. Caries of mastoid. Loud pistol-like report. Sensitive to noise. Roaring. Boils on gums. Abscess at root of teeth. Pyorrhea. Inguinal glands swollen and painful. Hepatic abscess. Fissures and haemorrhoids.
Bovista
Scurf and crusts about nostrils and corners of mouth. Lips chapped. Bleeding of nose and gums. Cheeks and lips feel swollen. Acne. Leucorrhea. Candidiasis. Eczema, moist; formation of thick crusts. Pimples cover the entire body; scurvy; herpetic eruptions. Pruritus ani. Urticaria.
Colic. Pain around umbilicus. Stitches through perineum towards rectum and genitals. Chronic diarrhea.
Calcarea Carbonica
Inflammation and swelling of the womb, with redness, purulent discharge, and burning pain. Candidiasis. Varices in the labia majora. Leucorrhea and vaginal candidiasis. Skin unhealthy; readily ulcerating; flaccid. Small wounds do not heal readily. Glands swollen. Nettle rash. Warts. Petechial eruptions. Chilblains. Boils. Burning, stinging hemorrhoids. Diarrhea of undigested food. Frequent sour eructations; sour vomiting. Dry, nostrils sore, ulcerated. Stoppage of nose, also with fetid, yellow discharge. Offensive odor in nose. Polypi; swelling at root of nose.
Hydrastis Canadensis
Candidiasis. Leucorrhea: tenacious, ropy, thick yellow. Ulceration of the os, cervix, and vagina; debility; prolapsus uteri. Os uteri very tender. Uterine hemorrhage; menorrhagia and metrorrhagia, with fibroid tumors; at menopause. Pruritus vulvae, with profuse leucorrhea; sexual excitement. Lancinating pain in breast extending up to shoulder and down arm.
Ozaena, with ulceration of septum. Peppery mouth taste. Tongue white, swollen, large, flabby, slimy; shows imprint of teeth. Follicular pharyngitis. Atonic dyspepsia. Ulcers and cancer. Gastritis. Gastro-duodenal catarrh. Liver torpid, tender. Jaundice. Gallstones. Rectal prolapsed, hemorrhoids.
Sulphur
Pudenda itches. Vagina burns. Offensive perspiration. Leucorrhea and vaginal candidiasis. Leucorrhea, burning, excoriating. Nipples cracked, smart and burn. Otorrhea. Oversensitive to odors. Deafness. Chronic ophthalmia, with burning and itching. Itching of genitals. Skin dry, scaly, unhealthy; every little injury suppurates. Freckles. Itching, burning. Pimply eruption, pustules, rhagades, hangnails. Excoriation, especially in folds. Feeling of a band around bones. Skin affections after allopathic medication. Pruritus 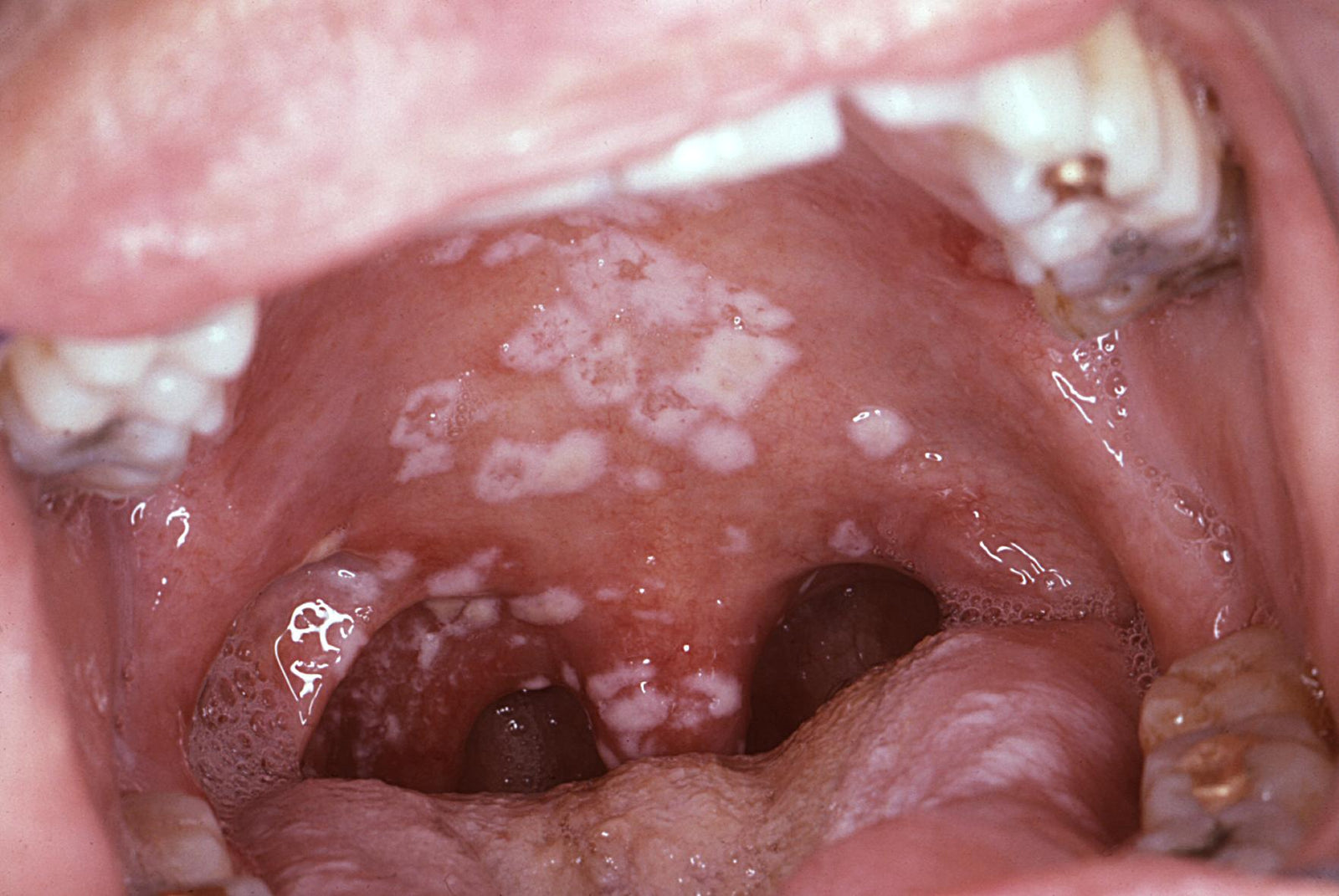
Herpes across the nose. Nose stuffed indoors. Imaginary foul smells. Alae red and scabby. Chronic dry catarrh; dry scabs, bleeding. Polypus and adenoids. Lips dry, bright red, burning. Bitter taste in morning. Swelling of gums; throbbing pain. Tongue white, with red tip and borders.
Throat burning, redness and dryness. Complete loss of, or excessive appetite. Putrid eructation. Food tastes too salty. Drinks much, eats little. Sever acidity, sour eructation. Burning, painful, weight-like pressure. Very weak and faint.
Graphites
Aversion to coitus. Vesicles and pimples on the vulva, excoriation on the vulva and between the thighs, vaginal soreness, ovarian swelling and pain after getting wet.
Dryness of the lids. Eczema of lids; fissured. Moisture and eruptions, fissure behind the ears. Scabs and fissures in nostrils. Moist eczema. Early stage of keloid and fibroma. Pimples and acne. Eruptions, oozing out a sticky exudation.
Swelling of the cheeks or of the feet, catarrh, with hoarseness and coryza, toothache, or cramps and violent cuttings in the abdomen, headache, nausea, pain in the chest, and weakness. Leucorrhea and vaginal candidiasis, white and liquid, like water, with tension of the abdomen, and weakness in the back. Before and after the catamenia leucorrhea, discharge occurs in gushes day or night. Painful sensibility and excoriation of the breasts, with eruption of running phlycten.
Mezereum
Chronic leucorrhea, like white of eggs (malignant, corroding), sometimes, menses are too frequent and lasting too long; scanty with leucorrhea and prosoplasia; suppressed. Leucorrhea and vaginal candidiasis. Soreness and burning in bones of thorax, constriction.
 Cutaneous ulcers with thick, whitish, yellow scabs, which thick, yellow pus. Miliary eruptions, sometimes chronic. Furunculi -Inflamed ulcers, with burning and shooting, or with gnawing pain, with an areola, sensitive and easily bleeding when removing the linen, which sticks, painful at night, the pus tends to form an adherent scab, under which a quantity of pus collects, burning and stinging with inflammation. Vesicles around the ulcers, itching violently and burning, like fire. Suppuration after inflammation.
Cutaneous ulcers with thick, whitish, yellow scabs, which thick, yellow pus. Miliary eruptions, sometimes chronic. Furunculi -Inflamed ulcers, with burning and shooting, or with gnawing pain, with an areola, sensitive and easily bleeding when removing the linen, which sticks, painful at night, the pus tends to form an adherent scab, under which a quantity of pus collects, burning and stinging with inflammation. Vesicles around the ulcers, itching violently and burning, like fire. Suppuration after inflammation.
Thuja Occidentalis
Thuja Occidentalis is a medicine for yeast infection or fungal infections that appear as ringworms in the beard, mustache, neck area or other hairy areas (tinea barbae).
Vagina very sensitive. Warty excrescences on vulva and perineum. Profuse thick, greenish leucorrhea. Severe pain in left ovary and left inguinal region. Menses scanty, retarded. Leucorrhea and vaginal candidiasis.
Polypi; fleshy excrescences. Polypi, tubercles, warts epithelioma, naevi, carbuncles; ulcers, especially in anogenital region. Freckles and blotches. Perspiration sweetish and strong, skin dry, with brown spots, zona; herpetic eruptions. Eruptions only on covered parts; worse after scratching. Very sensitive to touch. Coldness of one side. Sarcoma.
Borax
Leucorrhea, corrosive, and thick, like starch. Sterility. Acrid leucorrhea, appearing for two weeks between catamenia, with swelling of labia and inflamed and discharging Duvernay’s glands. Leucorrhea and vaginal candidiasis.
Stinging and distended feeling in clitoris. During pregnancy, swelling, itching, and burning of vagina, with a discharge like gonorrhea. False pains. Labour pains: spasmodic; more in stomach than in uterus; dart upwards, head of child goes back. Sterility; During pregnancy, swelling, itching, and burning of vagina, with a discharge like gonorrhea.
Skin difficult to heal; dingy, unhealthy skin; every injury tends to ulceration. Erysipelatous inflammations, with swelling and tension of the part affected, and fever. Whitish pimples, with red areola. Herpetic eruptions. Purulent and phagedenic vesicles.
Merc Solobus
Before catamenia: dry heat, with ebullition of blood, and congestion in head. Congestion of blood to
uterus. Inflammation of ovaries and uterus. Leucorrhea in general; complaints concomitant to leucorrhea like greenish discharge; smarting, corroding, itching, burning after scratching etc. Candidiasis.
Hard tubercles on labia majora. Itching pimples, and nodosities in labia. Itching of genitals. Furrow in upper surface of tongue lengthwise. Tongue heavy, thick; moist coating; yellow, flabby, teeth-intended, feels as if burnt, with ulcers, Fetid odor from mouth, can smell it all over room. Alveolar abscess.
Pulsatilla Pratensis
Contractive pain in uterus, like labor pains, Labour-pains too weak, spasmodic, or ceasing, obliging her to bend double. Spasmodic pains, or drawing tension in uterus, and pains like those of labor. After-pains in females of a mild disposition. Otorrhea with thick, bland, offensive discharges.
Urticaria. Orchitis; pain from abdomen to testicles. Thick, yellow discharge from urethra. Burning in orifice of urethra during and after micturition. Yellow or white tongue, covered with a tenacious mucus. Loss of smell. Large green fetid scales in nose. Thick, profuse, yellow, bland discharges from eyes.
A burning (sticking) pain in vagina and pudenda. Metrorrhagia (discharge now stopping, and then stronger again, of coagulated, clotted blood, or with false labor-pains). Menstrual blood black, with clots of mucus, or pale and serous.
Catamenia irregular, tardy, or premature, of too short or too long duration, or entirely suppressed (esp. if produced by getting the feet wet), with colic, hysterical spasms in abdomen, hepatic pains, gastralgia, pain in loins. Leucorrhea and vaginal candidiasis. Leucorrhea, thick, like cream (especially frequent in lochia discharges where the flow looks like milk), or corrosive and burning, principally at period of catamenia before, during or after), and sometimes with cuttings (better when lying down; with swollen vulva).
Zincum Metalicum
Catamenia premature and too copious. Suppressed menstruation, with full habit. Sterility and or Miscarriage voluptuous sensation in the genital parts, with emission. Metrorrhagia, Itching or pressing in the vagina, shootings in the orifice of the matrix, and pressive pain in the vagina, itching, Inflammation and swelling the womb with redness, purulent discharge, and burning pain. Varices in the labia majora. Leucorrhea before the catamenia, with burning itching, or else like milk, flowing by fits, and during the emission of urine. Candidiasis.
Eruption of lenticular red and raised spots, with great heat, much thirst, and want of appetite. Skin hot and dry as if covered with a kind of miliary eruption. Furfuraceous coating of the skin; burning; chapped. Pale lips, and corners of mouth cracked. Redness and itching eruption on chin.
Humid, scabby eruptions and titters, or in form of clusters, with burning pains. Itching pemphigus, Ulcers deep; fistulous; carious with too little pus. Erysipelatous inflammations. Furunculi, warts, corns, with pain as of excoriation, and burning. Polyps uterus. Constriction/spasmodic and cutting in chest. Eczema
Lilliam Tigrum
Acrid, brown leucorrhea; smarting in labia. Sexual instinct awakened. Bloated feeling in uterine
region. Subinvolution. Pruritus pudenda, Bearing down, with sensation of heavy weight and pressure in uterine region.
Voluptuous itching in vagina, with feeling of fullness of parts. Leucorrhea and vaginal candidiasis. Leucorrhea; bright yellow, acrid, excoriating; leaving a brown stain; after menses.
Menses continue only when moving about and cease when sitting or lying down. Amenorrhea.
Kreosotum
Premature catamenia, of too long continuance, and too copious, with a discharge of black blood. During an embrace, burning in the parts, followed next day by menstrual discharge of dark blood.
Before the catamenia, abdominal spasms, leucorrhea, irritation, and inquietude. After menses pressure in the genitals; leucorrhea; and many other sufferings. Metrorrhagia in fungoid disease of endometrium.
Leucorrhea and vaginal candidiasis. Corrosive or mild leucorrhea, and sometimes followed by exhaustion and fatigue, especially in legs. Leucorrhea of a yellow color, staining linen yellow.
White leucorrhea, having odor of green corn. Leucorrhea putrid, with accompanying complaints; leucorrhea in general, esp. if very fetid and exhausting.
Complaints of females at change of life. Cramp-like pains in external genitals. Excoriation, with smarting pains between genitals and thighs. Shootings in vagina, as if produced by electricity. Voluptuous itching in vagina, inducing rubbing in evening, succeeded by smarting, swelling, heat, and induration of external parts, with soreness in vagina when urinating.
Desire for coition, in females, especially in morning; after coition, pain, as of excoriation, and hard knottiness in neck of uterus, or swelling of the genital parts (both male and female) with burning pains (worse in morning than in evening).
After coition discharge of dark blood, the next day. Prolapses vaginae, prolapsus uteri.
Soft, unnatural feel of skin, violent itching all over, especially towards evening, and with burning sensation after scratching.
Arsenicum Album
Venereal desire in women. Catamenia too early and too copious, attended by much suffering. Catamenia suppressed, with pains in the sacrum and in the shoulders.
Leucorrhea and vaginal candidiasis. Leucorrhea acrid, corrosive, thick, and yellowish, scirrhous uteri.
Vesicular eruptions. Herpes, with vesicles, and violently burning, especially at night, or with coverings, like fish-scales, general anasarca; black blisters, pustules filled with blood and pus, titter spots, covered with phlyctenules and furfur, with burning nocturnal pains.
Inflammatory tumors with burning pains, warts. ulcers inform of a wart. Varices.
Cantharis
Catamenia premature and too copious, with black blood and pains during the flow. Voiding of moles, of fetus, and of placentae.
Female Sexual Organs. Catamenia premature and too copious, with black blood and pains during the flow. Voiding of moles, of fetes, and of placentae. Leucorrhea and vaginal candidiasis.
Inflammation of the ovaries. Swelling of the cervix uteri. Corrosive leucorrhea, with burning sensation on making water, and excitement of sexual desire.
Itching vesicles, with burning pain on being touched. Blisters, from burns. Erysipelatous inflammation. Acute drawing pains in ulcers, with increased suppuration.
Apis Mellifica
Abortion. Abortion during the early months. Dropsy in the latter part of pregnancy attended with puerperal convulsions. Erysipelatous inflammation of the breasts. Swelling and hardness of the mammae threatening to ulcerate. Scirrhous or open cancer of the mammae, with stinging, burning pains.
Amenorrhea or menorrhagia. Inflammation, induration, swelling, and dropsy of the ovaries (rite sided). Leucorrhea and vaginal candidiasis. Ovarian tumors, with stinging pains like bee stings. Metritis, peritonitis, with stinging, thrusting pains.
Pressing down or bearing down pain in the uterus, with sensation as before menses. Ulceration and engorgement of os uteri. Large and painful swelling of the labia, with heat and stinging pains.
Ovarian tumors, with stinging pains like bee stings. Threatened miscarriage in the early months. Metritis, peritonitis, with stinging, thrusting pains. Dropsy of the ovaries; dropsy of the uterus. Strained pain ovary.
Menstruation suppressed or diminished, with congestion to the head. Labour-like, bearing-down pains, followed by dark, bloody mucus, Ulceration and engorgement of os uteri. Large and painful swelling of the labia, with heat and stinging pains.
Natrum Muriaticum
Spitting blood at menstrual nisus; Itching in genital organs. Repugnance to coition. Coition: painful from dryness of vagina; burning smarting during; in anemic women with dry mouth and dry skin.
Leucorrhea and vaginal candidiasis with headache, disposition to diarrhea, colic, and mucous evacuations. Acrid (greenish) leucorrhea (increased discharge when walking), with yellow color of face. Abundant discharge of transparent, whitish, and thick mucus from vagina.
Vulvitis with falling off of hair. Itching of external parts with falling off of hair. Pimples on mons veneris.
Heper Sulphuricum
Urine voided slowly, without force-drops vertically, bladder weak. Seems as if some always remained. Greasy pellicle on urine. Bladder difficulties. Discharge of blood from uterus. Itching of pudenda and nipples, worse during menses. Menses late and scanty. Abscesses of labia with great sensitiveness. Extremely offensive leucorrhea. Smells like old cheese. Profuse perspiration at the climacteric. 
Sanicula Aqua
Bearing down, as if contents of pelvis would escape; better, rest. Desire to support parts. Soreness of uterus. Leucorrhea with odor of fish-brine or cold cheese. Vagina feels large. Dislocated feeling in sacrum. Burning of soles of feet. Offensive sweat. Cold, clammy sweat of extremities.
Tilia Europaea
Intense sore feeling about uterus; bearing down, with hot sweat. Much slimy leucorrhea when walking. Soreness and redness of external genitals. Pelvic inflammation, tympanites, abdominal tenderness and hot sweat.
Terebinthina or Oleum terebinthinae for leucorrhea or Vaginal Candidiasis
Catamenia retarded and scanty. Drawing in thighs and colic as if menses would set in, a week after she had had them. Uterus and ovaries very painful. Ovarian dropsy. Terrible burning in uterus, with great bearing-down pain; caused great heat all over; craves drink; inward heat. Uterine diseases after wearing pessaries. Fibroids; bloody leucorrhea; burning in uterus; menorrhagia, black blood. Leucorrhea and vaginal candidiasis.
Herpes labialis. Abortion. Neuralgia during pregnancy. Burning and bearing down in uterus during urination. Metritis, lochia checked, burning in uterus. Peritonitis after confinement from tight lacing.
Lycopodium Clavatum
Thick, yellow, offensive ear discharge. Eczema about and behind ears. Otorrhea and deafness with or without tinnitus; after scarlatina. Humming and roaring with hardness of hearing; every noise causes peculiar echo in ear.
Sense of smell very acute. Feeling of dryness posteriorly. Scanty excoriating, discharge anteriorly. Ulcerated nostrils. Crusts and elastic plugs. Itching; scaly herpes in face and corner of mouth. Teeth excessively painful to touch, with swelling of cheeks. Tongue dry, black, cracked, swollen; oscillates to and fro. Mouth waters. Blisters on tongue. Bad odor from mouth.
Dryness of throat, without thirst. Food and drink regurgitate through nose. Inflammation of throat, with stitches on swallowing. Swelling and suppuration of tonsils. Ulceration of tonsils, beginning on right side. Diphtheria. Ulceration of vocal bands. Tubercular laryngitis.
Dyspepsia. Sour eructation. Sever weakness of digestion. Bulimia, with much bloating. Rolling of flatulence. Immediately after a light meal, abdomen is bloated, full. Dropsy, due to hepatic disease. Hepatitis, atrophic from of nutmeg liver. Diarrhea. Inactive intestinal canal. Hemorrhoids.
Pain in back before urinating; ceases after flow; slow in coming, must strain. Retention. Polyuria during the night. Enlarge prostate. Condylomas.
Vagina dry. Coition painful. Leucorrhea, acrid, with burning in vagina. Discharge of blood from genitals during stool.
Tickling cough. Dyspnea. Tensive, constrictive, burning pain in chest. Expectorations gray, thick, bloody, purulent, salty. Neglected pneumonia.
Kalium Bichromicum
Supra-orbital neuralgia. Eyelids burn, swollen, edematous. Discharge ropy and yellow. Ulcers on cornea; no pain or photophobia. Descemetitis, with only moderate irritation of eye. Croupous conjunctivitis; granular lids, with pannus. Iritis, with punctuate deposits on inner surface of cornea. Slight pain, with severe ulceration or inflammation.
Thick, yellow, stringy, fetid discharge from ear. Septum ulcerated, round ulcer. Fetid smell. Discharge thick, ropy, greenish yellow. Tough, elastic plugs from nose; leave a raw surface. Inflammation extends to frontal sinuses, with distress and fullness at root of nose.
Mouth dry; viscid saliva. Tongue mapped, red, shining, smooth, and dry, with dysentery; broad, flat, indented, thickly coated. Feeling of a hair on tongue. Faucets red and inflamed. Dry and rough. Parotid glands swollen. Uvula relaxed, edematous, bladder-like. Pseudo-membranous deposit on tonsils and soft palate. Burning extending to stomach. Aphthae. Diphtheria. Discharge from mouth and throat, tough and stringy.
Gastritis. Round ulcer of stomach. Stitches in region of liver and spleen and through to spine. Vomiting of bright yellow water. Chronic intestinal ulceration. Soreness in right hypochondrium, fatty infiltration of liver and increase in soft fibrous tissue. Painful retraction, soreness and burning. Stool: Jelly-like, gelatinous; worse, mornings. Dysentery: tenesmus, stools brown, frothy.
Burning in urethra. After urinating a drop seems to remain which cannot be expelled. Ropy mucus in urine. Congestion of kidneys; nephritis, with scanty, albuminous urine and casts. Itching and pain of penis, with pustules. Ulcers, with paroxysmal stitches. Constriction at root of penis. Syphilitic ulcers, with cheesy, tenacious exudation.
Yellow, tenacious leucorrhea. Pruritus of vulva, with great burning and excitement. Prolapsus uteri; worse in hot weather.
Skin: Acne. Papulas eruptions. Ulcer with punched-out edges, with tendency to penetrate and tenacious exudation. Pustular eruption, resembling smallpox, with burning pains. Itching with vesicular eruption.
Acid Muriaticum
Tongue, pale, swollen, dry, leathery, paralyzed. Deep ulcers on tongue. Hard lumps in tongue. Epithelioma; edges bluish red. Aphthous mouth. Gums and glands swollen. Fetid Breath. Sores on teeth. Uvula swollen. Ulcers and false membrane. Edematous, dark, raw. Attempted swallowing produces spasm and choking.
Tendency to involuntary evacuations while urinating. Hemorrhoid most sensitive to all touch; even sheet of toilet paper is painful. Anal itching and anal prolapsus while urinating. Hemorrhoid bluish, hot with violent stitches.
Menses appear too soon. Leucorrhoea. During menses, soreness of anus. Ulcer in genitals.
Acid Nitricum
Blisters and ulcers in mouth, tongue, genitals; bleed easily. Fissures, with pain during stool, as if rectum were torn. All discharges very offensive, especially urine, feces, and perspiration. Double vision; sharp, sticking pains. Ulceration of cornea. Gonorrheal ophthalmia, photophobia, constant lachrymation. Syphilitic iritis.
Nose: Ozaena. Green casts from nose every morning. Coryza, with sore and bleeding nostrils. Tip red. Stitches. Caries of mastoid. Nosebleed, with chest affections. Chronic nasal catarrh, with yellow, offensive, corrosive discharge. Nasal diphtheria, with watery and exceedingly excoriating discharge.
Putrid breath. Salivation. Bleeding of gums. Painful pimples on the sides of the tongue. Tongue clean, red and wet with center furrow. Teeth become loose, gums soft and spongy. Ulcers in soft palate, with sharp, splinter-like pains. Salivation and fetor oris. Bloody saliva. Throat dry. Pain into ears. Hawks mucus constantly. White patches and sharp points, as from splinters, on swallowing. Pain in cardiac orifice. Dyspepsia. Fissures in rectum. Tearing violent cutting pains after stools, lasting for hours. Jaundice, aching in liver.
Male: Soreness and burning in glans and beneath prepuce. Ulcers; burn and sting; exude, offensive matter.
Female: External parts sore, with ulcers. Leucorrhea brown, flesh-colored, watery, or stringy, offensive. Hair on genitals falls out. Uterine hemorrhages. Stitches through vagina. Metrorrhagia after parturition.
Warts, large jagged; bleed on washing. Ulcers bleed easily, sensitive; splinter-like pains; zigzag, irregular edges; base looks like raw flesh. Exuberant granulations. Black pores on face, papules worse on forehead.
Natrium Phosphoricum
Canker sores of lip and cheeks. Blisters on tip of tongue. Thin, moist coating on the tongue. Yellow, creamy coating at the back part of the roof of the mouth. Dysphagia. Thick, creamy membrane over tonsils and soft palate. Sour eructation, sour vomiting, greenish diarrhea.
Menses too early; pale, thin, watery. Sterility, with acid secretions from vagina. Leucorrhea; discharge creamy or honey-colored, or acid and watery. Sour-smelling discharges from uterus. Morning sickness, with sour vomiting.
Skin yellow. Itching in various parts, especially of ankles. Hives. Smooth, red, shining. Erysipelas. Feet icy cold in daytime, burn at night. Swelling of lymphatic glands.
Natrium Sulphuricum
Nasal catarrh, with thick, yellow discharge and salty mucus. Coryza. Epistaxis. Ethmoiditis. Conjunctiva yellow. Granular lids. Photophobia. Slimy, thick, tenacious, white mucus in mouth. Bitter taste, blisters on palate.
Throat: Thick, yellow mucus drops from posterior nares.
Vomits sour. Brown, bitter coating on tongue. Bilious vomiting, acid dyspepsia, with heartburn and flatulence. Duodenal catarrh; hepatitis; icterus and vomiting of bile; liver sore to touch, with sharp, stitching pains; cannot bear tight clothing around waist. Flatulency; wind colic in ascending colon. Burning in abdomen and anus. Bruised pain and urging to stool. Diarrhea yellow, watery stools. Loose morning stools, worse, after spell of wet weather. Stools involuntary, when passing flatus. Great size of the fecal mass.
Herpetic vulvitis. Leucorrhea yellowish green, following gonorrhea in female. Leucorrhea with hoarseness.
Male: Condylomas; soft, fleshy excrescences; greenish discharges. Gonorrhea; discharge thick, greenish; little pain.
Itching while undressing. Jaundiced, watery blisters. Sycotic excrescences; wart-like red lumps all over body.
P. S: This article is only for doctors and students having good knowledge about Homeopathy and allopathy.

For proper consultation and treatment, please visit our clinic.
 Dr. Sayyad Qaisar Ahmed (MD {Ukraine}, DHMS), Abdominal Surgeries, Oncological surgeries, Gastroenterologist, Specialist Homeopathic Medicines.
Dr. Sayyad Qaisar Ahmed (MD {Ukraine}, DHMS), Abdominal Surgeries, Oncological surgeries, Gastroenterologist, Specialist Homeopathic Medicines.
Senior research officer at Dnepropetrovsk state medical academy Ukraine.
Location: Al-Haytham clinic, Umer Farooq Chowk Risalpur Sadder (0923631023, 03119884588), K.P.K, Pakistan.
Find more about Dr Sayed Qaisar Ahmed at:
https://www.youtube.com/Dr Qaisar Ahmed



