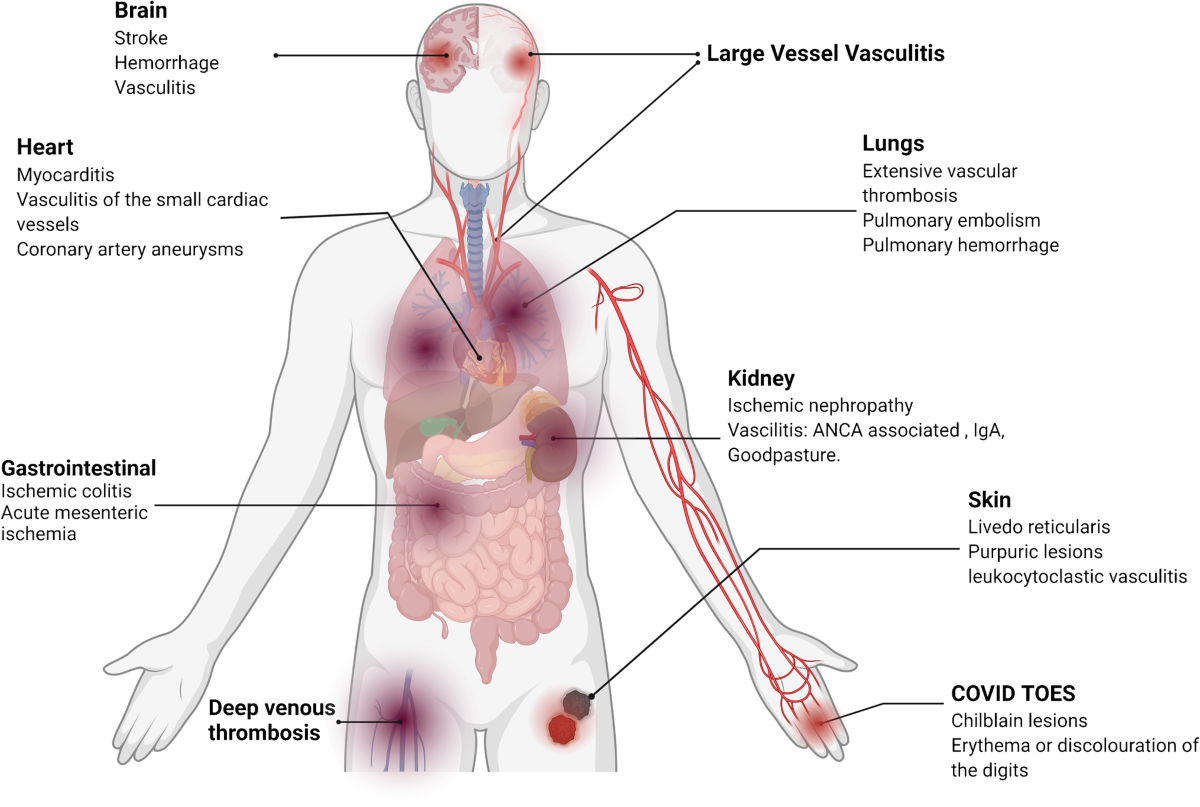
Vasculitis is a heterogeneous group of pathologies characterized by inflammation of vessels and is defined as inflammation of blood vessels. It may result in vessel wall thickening, stenosis, and occlusion with subsequent ischemia. Necrotizing inflammation can completely destroy segments of the wall. Vasculitis can involve vessels of any size and can affect any organ system. The clinical presentation varies according to the histologic type of inflammation, the size of the involved blood vessel segment, and the distribution of the involved vessels.
They share common links of clinical, laboratory, and pathophysiologic features. The clinical and pathological features are variable and depend on the site and type of blood vessels affected.
Types of vasculitis
Research has identified more than 30 kinds of vasculitis. Vasculitis may present as a primary process or secondary to another underlying disease. Diseases in which vasculitis is a primary process are called primary systemic vasculitis.
Symptoms
Vasculitis symptoms and signs vary greatly and depend upon the organs affected and the severity of the disease, for example:
Cause of vasculitis
Researchers don’t know the cause of vasculitis; however, common features of the condition include inflammation of blood vessels and immune system abnormalities. Examples of diseases and conditions in which vasculitis occurs include: 
- Kawasaki disease,
- Behçet’s disease,
- Polyarteritis nodosa,
- Granulomatosis with polyangitiis,
- Churg-Strauss syndrome,
- Temporal arteritis (giant cell arteritis),
- Henoch-Schönlein purpura,
- Vasculitis also may occur with infections, drugs (cocaine, amphetamines), cancers, lupus, and rheumatoid arthritis etc.
Specific Classification Criteria
Large vessel vasculitis
Note that the main large vessel vasculitis that affects children is Takayasu arteritis (its vasculitis -granulomatous inflammation of the aorta and its major branches), and that temporal arteritis is not seen in the pediatric population.
Takayasu arteritis is characterized by transmural inflammation and evidence of intramural giant cells. It involves the aorta and its major branches. Characteristic clinical features are caused by stenotic large vessels and subsequently decreased blood supply to the organ systems. Classically, children present with claudication, absent peripheral pulses, blood pressure abnormalities, strokes, and features of internal organ ischemia. Prevalence of stroke/transient ischemic attack in patients with Takayasu arteritis of almost 16%.
Classification criteria for Takayasu arteritis includes angiographic abnormalities (conventional, CT, or MRI) of the aorta or its main branches (mandatory criterion), plus at least one of the following features:
- Decreased peripheral artery pulse and/or claudication of extremities,
- Blood pressure difference of more than 10 mm Hg,
- Bruits over aorta and/or its major branches,
- Hypertension (related to childhood normative data).
Medium-vessel vasculitis
The most common childhood medium-vessel vasculitis is Kawasaki disease. It is a necrotizing vasculitis that has a predilection for the coronary arteries. Classic features include prolonged fever, mucocutaneous changes and lymphadenopathy. Other manifestations may include irritability, arthritis, and abdominal pain.
Classification criteria for Kawasaki disease include a fever persisting for at least five days (mandatory criterion) plus 4 of the following 5 features:
- Changes in peripheral extremities or perineal area,
- Polymorphous exanthema,
- Bilateral conjunctival injection,
- Changes of lips and oral cavity (injection of oral and pharyngeal mucosa),
- Cervical lymphadenopathy.
Childhood polyarteritis nodosa is a necrotizing vasculitis of medium-sized arteries and is recognized in distinct systemic and cutaneous forms.
Systematic nodosa
Systemic polyarteritis nodosa involves all organ systems and the presentation widely varies. Features include vasculitic skin lesions, hypertension, neuropathy, and myalgia. Note that renal involvement does not manifest as glomerulonephritis, as occurs with small-vessel disease. Unlike in adults, angiographic or biopsy evidence of vasculitis is required to make this diagnosis.
Classification criteria for polyarteritis nodosa include a systemic illness characterized by the presence of either a biopsy finding that reveals small and mid-size artery necrotizing vasculitis or angiographic abnormalities (aneurysms or occlusions), plus at least 2 of the following:
- Skin involvement (eg, livedo reticularis, tender subcutaneous nodules, other vasculitic lesions),
- Myalgia or muscle tenderness,
- Systemic hypertension, relative to childhood normative data,
- Mononeuropathy or polyneuropathy,
- Abnormal urine analysis and/or impaired renal function (glomerular filtration rate of < 50% normal for age),
- Testicular pain or tenderness.
Signs or symptoms suggesting vasculitis of any other major organ system (GI, cardiac, pulmonary, CNS). 
Cutaneous polyarteritis nodosa is characterized by the presence of subcutaneous nodular, painful, nonpurpuric lesions with or without livedo reticularis and absence of systemic involvement. However, more than half of patients also have myalgia, arthralgia, and nonerosive arthritis. Cutaneous polyarteritis nodosa has been associated with serological or microbiological evidence of streptococcal infection in 40% of patients.
Childhood PACNS is defined by clinical evidence of a newly acquired focal or diffuse neurologic deficit plus angiographic or histologic evidence of CNS vasculitis, in the absence of a systemic condition associated with these findings.
Two clinically and radiologically distinct types of childhood PACNS are noted: large-medium vessel (angiography-positive) and small vessel (angiography-negative).
Small-vessel vasculitis
Henoch-Schönlein purpura (the most common vasculitis in children) is associated with immunoglobulin A (IgA) immune deposition in small vessels. Presenting features include palpable purpura, abdominal pain (which may be associated with GI hemorrhage and/or intussusception), arthritis, and evidence of glomerulonephritis (hematuria, proteinuria).
Classification criteria for Henoch-Schönlein purpura include palpable purpura (mandatory criterion) in the presence of at least one of following 4 features:
- Diffuse abdominal pain,
- Any biopsy finding that reveals predominant lgA deposition,
- Arthritis or arthralgia (arthritis is acute in any joint),
- Renal involvement (any hematuria, proteinuria).
ANCA
Antineutrophil cytoplasmic antibody (ANCA) positive small-vessel vasculitis are also seen in the pediatric population. Granulomatosis with polyangiitis (GPA) (formerly known as Wegener granulomatosis) is a granulomatous vasculitis that most commonly involves the sinopulmonary system but can involve any organ system. Presenting features may include purpuric rash, recurrent sinusitis, epistaxis, shortness of breath, and/or hemoptysis from alveolar hemorrhage. It is also commonly associated with a necrotizing glomerulonephritis that may cause significant renal impairment. Patients with Wegener granulomatosis have a positive ANCA finding in 90% of cases, most frequently in a cytoplasmic pattern (c-ANCA), with antibodies against proteinase 3 (anti-PR3).
Classification criteria for GPA include 3 of the following 6 features: 
- Abnormal urinalysis findings (hematuria and/or significant proteinuria),
- Granulomatous inflammation on biopsy (If a kidney biopsy is done it characteristically shows necrotizing pauci-immune glomerulonephritis),
- Nasal sinus inflammation,
- Subglottic, tracheal, or endobronchial stenosis,
- Abnormal chest radiography or CT findings,
- PR3 ANCA or c-ANCA staining.
Microscopic polyangiitis (MPA) is a necrotizing vasculitis associated with glomerulonephritis and pulmonary capillaritis. Presenting features include purpuric rash, proteinuria and/or hematuria, hemoptysis, CNS involvement, and arthralgias. MPA is associated with ANCA, most commonly with a perinuclear pattern (p-ANCA) and antibodies against myeloperoxidase (anti-MPO).
Churg srrauss syndrome
Churg-Strauss syndrome (CSS) is an eosinophilic granulomatous vasculitis characterized predominantly by pulmonary involvement. Patients typically have a previous history of asthma, allergic rhinitis, and/or sinusitis. A characteristic feature is the finding of nonfixed pulmonary infiltrates. Eosinophilic infiltration results in multiorgan involvement, including neuropathy and cardiovascular disease (pericarditis). ANCA positivity is seen in approximately 40% of patients, usually with an “atypical” or “indeterminate” pattern.
Isolated cutaneous-leukocytoclastic
Isolated cutaneous leukocytopclastic vasculitis can be either primary (rarely) or secondary to various medications, infections, or collagen vascular disease.
Hypocomplemeteric
Hypocomplementemic urticarial vasculitis is a cutaneous vasculitis that may result from primary hypocomplementemia or as part of a disease associated with low complement levels (eg, systemic lupus erythematosus).
Other vasculitis
Behcet disease involves vessels of all sizes. The diagnosis is made clinically in patients with recurrent oral ulcers who also have recurrent genital ulcers, uveitis, various skin lesions, and/or a positive pathergy test.
Anti-GBM antibody disease/Goodpasture syndrome is a type of vasculitis caused by deposition of anti-GBM antibodies in small vessels of lungs and kidneys. Goodpasture syndrome clinically manifests with rapidly progressive glomerulonephritis and/or pulmonary hemorrhage (pulmonary renal syndrome).
Thrombophlebitis
Thrombophlebitis refers to inflammation of a vein associated with the formation of a blood clot. This may arise due to an interaction of endothelial injury, stasis of blood, and a hypercoagulable state. Risk factors include intravenous catheter placement, immobilization, malignancy, inherited prothrombotic condition (eg, factor V Leiden, antithrombin III deficiency), antiphospholipid antibody syndrome, and Behçet disease. One study found vascular involvement in 14% of patients with Behçet disease, most commonly manifesting as superficial vein thrombophlebitis or deep vein thrombosis.
Pathophysiology
Vessel inflammation occurs by various mechanisms in this heterogenous group of diseases. The histopathological pattern of inflammation is a characteristic feature of the vasculitis subtypes. 
Lymphocytic/giant cell-mediated vasculitis
Takayasu arteritis and temporal arteritis (in adults) both involve large elastic arteries and share a similar histopathology. This form of vasculitis is T-cell dependent, and CD4+ T cells are the main players in the process. Dendritic cells within the arterial adventitia recruit and stimulate the CD4+ cells, which then activate the monocytes and macrophages that mediate oxidative injury of the vessel wall. Vascular lesions are characterized by a panarteritis with mononuclear infiltration of all layers of the arterial wall. Typically, activated T cells and macrophages are arranged in granulomas, and multinucleated giant cells are present. Often, the intimal layer is hyperplastic, leading to concentric occlusion of the lumen. Also, the end stage of giant-cell aortitis may be complicated by the formation and rupture of aneurysms.
Necrotizing vasculitis
Kawasaki disease and polyarteritis nodosa are examples of necrotizing vasculitis. Possible etiologies in the case of Kawasaki disease include infectious agents and/or superantigen-mediated activation of lymphocytes. The inciting factors in polyarteritis nodosa are less well understood; however, in developing countries, it has been associated with hepatitis B or C. Pathologically, segmental transmural inflammation of muscular arteries is noted. Nodule (vascular narrowing) and aneurysm formation result from panmural fibrinoid necrosis. Note that aneurysmal dilatation of the arterial wall is a common feature of necrotizing vasculitis. Typically, immunofluorescence for immunoglobulin or complement deposition is negative.
Antibody-mediated vasculitis
A review by Jennette and Falk discusses the scientific evidence showing that ANCA immunoglobulin Gs (IgGs) are involved in the pathogenesis of small vessel vasculitides such as GPA and MPA.
ANCA antibodies are directed towards cytoplasmic proteins within neutrophils and monocytes (eg, PR3, MPO), which may also be expressed at the cell surface, particularly on stimulated cells. In vitro studies have shown that ANCA IgGs can directly activate neutrophils and monocytes by both Fc receptor engagement and direct Fab2 binding to antigen. These activated cells interact with endothelial cells via adhesion molecules and release inflammatory mediators, such as toxic granule enzymes and reactive oxygen metabolites that cause apoptosis and necrosis.
In addition, anti-MPO IgG may activate MPO itself triggering an oxidative burst and resulting in severe endothelial damage. ANCA-activated neutrophils may release factors that activate the alternative complement pathway, which initiates an amplification loop that mediates the severe necrotizing inflammation of ANCA disease.
Antibody deposition
Henoch-Schönlein purpura is generally characterized by the deposition of IgA antibodies in affected tissues. Histopathologically, the typical finding on skin biopsy is leukocytoclastic vasculitis, with perivascular accumulation of neutrophils and mononuclear cells. Immunofluorescence demonstrates IgA, C3, and fibrin in the walls of affected vessels, including the postcapillary venules within the dermis, and the endothelial and mesangial cells of the kidney. Elevated serum IgA and circulating IgA-containing immune complexes may be present in some patients. One study showed that galactose deficiency of O-linked glycans in the hinge region of IgA1 has been associated with Henoch-Schönlein purpura. 
In anti-GBM antibody disease, circulating antibodies bind to type IV collagen within the glomerular basement membrane. Immunofluorescence study of renal biopsies demonstrates linear deposition of IgG along the glomerular basement membrane. Pulmonary hemorrhage occurs when these antibodies have access to the alveolar basement membrane.
Etiology
Secondary vasculitis
Infectious causes include the following:
- Tuberculosis,
- Streptococcus,
- Mycoplasma infections,
- Syphilis,
- HIV Infection,
- Herpes simplex,
- Varicella,
- Epstein-Barr virus (EBV),
- Cytomegalovirus (CMV),
- Parvovirus B19,
- Hepatitis B and C,
- Candida albicans.
Systemic diseases
Systemic rheumatic disease causes include the following:
- Systemic lupus erythematosus,
- Sjogren syndrome,
- Sarcoidosis,
- Juvenile dermatomyositis,
- Inflammatory bowel disease,
- Lemierre syndrome is an anaerobic suppurative thrombophlebitis of the internal jugular vein and is most commonly a complication of pharyngeal, dental, or mastoidal infection,
- Hypocomplementemic urticarial vasculitis is also a cause.
Malignancy causes include the following:
- Leukemia,
- Lymphoma,
- Bronchopulmonary blastoma, Angio blastoma (both rare).
Hypersensitivity vasculitis (leukocytoclastic vasculitis) and drug-induced ANCA vasculitis (propylthiouracil, hydralazine) are also both noted. 
Epidemiology
International statistics
In Japan, the incidence of Kawasaki disease is 188 per 100,000 children per year.
The global incidence of Henoch-Schönlein purpura is 10-20 cases per 100,000 children per year.
Race-, sex-, and age-related demographics
Race
The vasculitis is seen in patients of all races and ethnicities, but some notable patterns of distribution are noted.
- Kawasaki disease is most common in children of Japanese and other Asian descent.
- Henoch-Schönlein purpura is more common in Whites.
- Takayasu arteritis is more common in the Asian population.
- Behçet disease is more common in Turkey, the Middle East and eastern Asia.
Sex
- Henoch-Schönlein purpura has a male-to-female ratio of 2:1.
- Kawasaki disease has a male-to-female ratio of 1.6:1.
- Polyarteritis nodosa has a slight male preponderance.
- Takayasu arteritis has a strong female preponderance.
Age
- Henoch-Schönlein purpura has a peak age of onset at 3-10 years; 75% of patients are younger than 10 years.
- Kawasaki disease has a mean age of onset 4.3 years; 80% of patients are younger than 5 years.
- Polyarteritis nodosa has a peak age of onset at 9-11 years.
- Takayasu arteritis most commonly presents in the second and third decades of life; 20% are younger than 20 years.
Complications
Complications may include the following:
- Destruction of paranasal sinuses,
- Subglottic stenosis requiring tracheostomy,
- Life-threatening pulmonary hemorrhage,
- Renal insufficiency requiring dialysis or transplant,
- Digital gangrene with autoamputation,
- Stroke,
- Myocardial infarction,
- Sepsis,
- Morbidity associated with immunosuppressive medications,
- Death.
History
As vasculitis are systemic processes, a comprehensive history and full review of systems is necessary.
Possible triggers include the following: 
- Recent infections (upper respiratory tract infections, especially streptococcal; tuberculosis [TB]),
- Vaccinations – Eg, an Italian study found evidence that the measles-mumps-rubella (MMR), vaccine increases the risk of Henoch-Schönlein purpura (odds ratio = 3.4),
- New medications.
Presenting features include the following:
Constitutional
Constitutional symptoms – Fever, weight loss, fatigue, malaise (these occur in 90-100% of patients with granulomatosis with polyangiitis [GPA], formerly Wegener granulomatosis) and microscopic polyangiitis [MPA].
Skin
Nodules, which may be painful, erythematous, or ulcerated; purpura; petechiae; papulopustular lesions; erythema nodosum; livedo reticularis; Raynaud phenomenon; lower extremity swelling. Recurrent oral and/or genital ulcerations that heal with scarring.
Respiratory
Nasal/sinus – Allergic rhinitis, nasal congestion, recurrent epistaxis, sinus pain, tearing. Pulmonary – Chronic cough, hemoptysis, shortness of breath, stridor, wheezing, chest pain.
Musculoskeletal
Joint pain or swelling, myalgias, calf pain.
Urinary tract and genital
Renal – Hematuria, hypertension. Testicular swelling and/or pain.
GI tract
Abdominal pain, hematochezia, vomiting, nausea.
Vascular
Extremity claudication, blood pressure difference between limbs, pre-syncope/fainting spells.
Neurological
Headache, seizure, focal neurological deficits (eg, stroke, cranial nerve palsy, vision loss, fine motor deficits, movement abnormalities), diffuse neurological deficits (eg, cognitive decline, poor school performance), mononeuropathy or polyneuropathy (eg, numbness, paresthesia, hand/foot drop, weakness), visual/auditory hallucinations, fluctuating/decreased level of consciousness/encephalopathy. 
Past medical history may include the following:
- Recurrent sinusitis and pneumonias,
- Asthma and allergic rhinitis precede development of Churg-Strauss syndrome.
Family history may include an increased risk of Kawasaki disease in siblings.
Symptoms of Henoch-Schönlein purpura
Clinical features common in Henoch-Schönlein purpura include the following:
- Palpable purpuric rash (must be present),
- Diffuse abdominal pain,
- Arthritis (acute, any joint) or arthralgia,
- Hematuria and/or proteinuria,
- Lower limb swelling may be seen.
Symptoms of Kawasaki disease
Clinical features common in Kawasaki disease include the following:
- Fever, at least 5 days in duration, unresponsive to antibiotic therapy,
- Polymorphous exanthem (nonvesicular),
- Perineal desquamation,
- Changes in peripheral extremities (erythema and/or edema),
- Cervical lymphadenopathy, usually unilateral, larger than 1.5 cm,
- Bilateral, non-purulent, conjunctivitis,
- Changes of lips and oral cavity – Injection of oral and pharyngeal mucosa, fissured lips,
- Irritability, arthralgia/arthritis.
Physical Examination
General
Vital sign measurements should include 4-limb blood pressure measurement to look for a difference of more than 10 mm Hg between limbs.
Head and Neck
Fundoscopy and ophthalmologic assessment for conjunctivitis, uveitis, scleritis and/or retinal vasculitis, and optic neuritis is indicated. Orbital inflammation (lid edema/erythema, proptosis) may be seen in granulomatosis with polyangiitis and microscopic polyangiitis.
Inspection of nasal cavity for bleeding, ulceration, and septal perforation is indicated.
Other findings may include the following:
Arthritis (joint swelling, effusions, decreased range of motion and/or stress pain)
- Abdominal tenderness (focal or diffuse),
- Hepatomegaly, splenomegaly,
- Blood on rectal examination,
- Genital ulcers or scars in Behçet syndrome,
- Testicular pain and/or swelling,
- Muscle tenderness.
Nasal bridge swelling, pain or saddle-nose deformity
- Paranasal sinus tenderness,
- Cervical lymphadenopathy,
- Oral ulcers seen in Behçet disease,
- Otitis, mastoiditis, hearing loss.
Respiratory
- Increased work of breathing, tachypnea, hypoxia,
- Decreased breath sounds,
- Stridor, wheeze,
- Blood-tinged sputum.
Cardiovascular
The following may be noted:
- Pulselessness, inequality of pulses,
- Bruits over major arteries,
- Increased capillary refill time,
- Abnormal heart sounds, including gallop rhythm, muffled heart sounds, rub
Abdominal and genitourinary
Findings may include the following:
Dermatologic
Laboratory Studies
Investigations must be performed to detect signs of inflammation, to determine the type and extent of organ involvement, to test for vasculitis-specific autoantibodies, and to rule out secondary causes. Note that the degree of inflammation often differs between diseases and among individual patients.
General laboratory tests
- CBC count and differential may reveal normochromic, normocytic anemia; leukocytosis; thrombocytosis consistent with inflammatory process; and eosinophilia in Churg-Strauss syndrome.
- Erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP) may be elevated, but these findings are not sensitive or specific.
- C3 and C4 levels are usually elevated, except in hypocomplementemic urticarial vasculitis.
- Albumin levels may be low due to chronic inflammation, third spacing, or vascular leakage.
- von Willebrand factor antigen (factor VIII-related antigen) may be elevated.
Organ-specific tests
- BUN, creatinine, liver enzyme levels may be abnormal, depending on involvement.
- Urine studies for hematuria and/or proteinuria are indicated.
- Lumbar puncture may reveal pleocytosis, elevated protein levels, and/or elevated opening pressure in childhood primary angiitis of the CNS (PACNS)
Autoantibody tests
- The initial test for antineutrophil cytoplasmic antibody (ANCA) is indirect immunofluorescence to detect staining pattern, either cytoplasmic or perinuclear.
- If positive results are noted, test for reactivity to proteinase 3 (PR3) and myeloperoxidase (MPO) by enzyme-linked immunoassay (ELISA)
- ANCA positivity is noted in approximately 90% of pediatric patients with granulomatosis with polyangiitis (GPA) (formerly Wegener granulomatosis), 79% of whom are cytoplasmic.
- PR3-ANCA and MPO-ANCA positivity have a high sensitivity and specificity for the diagnosis of GPA and microscopic polyangiitis (MPA), respectively.
- The association of Churg-Strauss syndrome and ANCA positivity is approximately 40%.
Note that an atypical ANCA finding is nonspecific and may be seen in other inflammatory conditions such as infection and inflammatory bowel disease.
- Anti-glomerular basement membrane (GBM) antibody testing is indicated for pulmonary renal syndromes.
- Other autoantibodies such as anti-nuclear antibody (ANA) and rheumatoid factor (RF) are rarely positive. 
Infectious work-up (as indicated)
- Bacterial – Mycoplasma PCR and serology, antistreptolysin O test (ASOT), syphilis serology, Mantoux skin test,
- Viral – Serology for hepatitis B and C, parvovirus B19, HIV, herpes simplex virus, Epstein-Barr virus (EBV), cytomegalovirus (CMV), varicella,
- Fungal culture.
Thrombophilia investigations
Antiphospholipid antibody syndrome studies include the following: [30]
- Prolonged activated partial thromboplastin time (aPTT), which does not correct with mixing,
- Screening for lupus anticoagulant,
- Anticardiolipin antibody by ELISA,
- Anti-β2-microglobulin-1 antibody by ELISA.
Classification criteria for pediatric antiphospholipid antibody syndrome includes the following clinical criteria for vascular thrombosis:
One or more clinical episodes of arterial, venous, or small-vessel thrombosis, in any tissue or organ. Thrombosis must be confirmed by objective validated criteria (ie, unequivocal findings of appropriate imaging studies or histopathology).
For histopathologic confirmation, thrombosis should be present without significant evidence of inflammation in the vessel wall.
Lab criteria
The laboratory criteria include the following:
- Anticardiolipin antibody of immunoglobulin G (IgG) and/or immunoglobulin M (IgM) isotype in serum or plasma – Must be present in medium or high titre (ie, >40 GPL or MPL, or >99th percentile) on two or more occasions, at least 12 weeks apart, measured by a standardized ELISA,
- Anti-β2 glycoprotein-I antibody of IgG and/or IgM isotype in serum or plasma – Must be present in titre >99th percentile, on two or more occasions, at least 12 weeks apart, measured by a standardized ELISA,
- Lupus anticoagulant in plasma – Must be present on two or more occasions at least 12 weeks apart, detected according to the guidelines of the International Society on Thrombosis and Hemostasis.
Pediatric antiphospholipid syndrome is considered to be present if the clinical criterion and at least I of the laboratory criteria are met.
Other thrombophilia work-up includes protein C, protein S, antithrombin III, factor V Leiden mutation, homocysteine, prothrombin gene mutation (G20210A), and methylene tetrahydrofolate reductase (MTHFR) mutation.
Imaging Studies
Imaging is essential for evaluation of blood vessels and of end-organ damage. In particular, vascular imaging is often imperative for diagnosis and follow-up of the disease. Information regarding both luminal blood flow and vessel wall changes is important. Conventional angiography generally provides information about blood flow, clot formation, and collateral blood flow, whereas CT and/or magnetic resonance (MR) angiography provide visualization of vessel wall thickness and fragility, aneurysm formation, and overall disease activity.
End-Organ Imaging
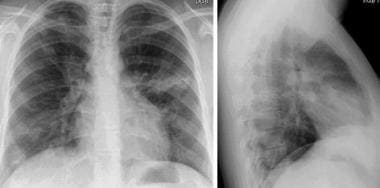
Chest radiography
This is indicated to screen for pulmonary involvement in granulomatosis with polyangiitis (formerly Wegener granulomatosis), Churg-Strauss syndrome, microscopic polyangiitis, Takayasu arteritis (TA), and Behçet syndrome.
A characteristic of CSS is fluctuating infiltrates. Chest radiography in Churg-Strauss syndrome (CSS) with pulmonary infiltrates.
CT scan of the sinuses
Turbinate mucosal thickening with associated sinusitis and possible erosive changes is seen in granulomatosis with polyangiitis.
 CT of sinuses in a patient with Wegener granulomatosis (WG) showing erosion and loss of sinus walls.
CT of sinuses in a patient with Wegener granulomatosis (WG) showing erosion and loss of sinus walls.
Orbital pseudotumor may be seen in granulomatosis with polyangiitis and microscopic polyangiitis.
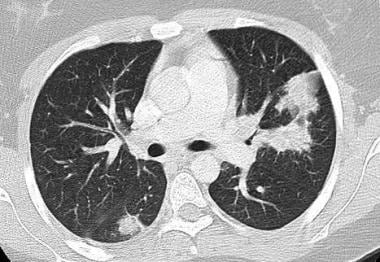
CT scan of the chest
In granulomatosis with polyangiitis, nodules (may be cavitary and/or multifocal), ground-glass opacification, air-space opacification, mediastinal lymphadenopathy, and pleural thickening and effusion may be seen.
In Churg-Strauss syndrome, nodules, ground-glass opacification, bronchial wall thickening or dilatation, consolidation, septal thickening, and tree-in-bud pattern may be seen.
In microscopic polyangiitis, patchy or confluent bilateral areas of consolidation may be seen, mainly in lower lobes.
Echocardiography
Echocardiography is indicated to assess for coronary artery involvement, especially in Kawasaki disease (KD).
Head CT scan or MRI
These studies may reveal acute ischemia or hemorrhage in patients with CNS symptoms. In large or medium-vessel childhood PACNS, T2-hyperintense focal areas of acute ischemia in a vascular distribution is noted. Diffusion weighted imaging (DWI) findings are positive. Vessel wall enhances with gadolinium.
In small-vessel childhood PACNS, T2-fluid-attenuated inversion-recovery (FLAIR) hyperintensities that do not conform to a vascular territory are noted. DWI findings are negative.
Vascular Imaging
CT angiography, MR angiography, or conventional angiography plus MRI vessel wall imaging (gadolinium enhancement)
These studies are used to assess for large and/or medium vessel vasculitis:
Angiography (CT, MR, conventional) of the aorta and its main branches is indicated when investigating for Takayasu arteritis.
Head MR angiography is diagnostic in large/medium vessel childhood PACNS.
PAN imaging
Vascular imaging in polyarteritis nodosa (PAN) must be done with conventional angiography because medium-sized vessels are involved (site depends on clinical features); findings include “beading” of vessels caused by alternating areas of vascular narrowing and dilatation.
Consider angiography in Behçet disease (site depends on clinical features).
CT/MR venography is indicated if venous thrombosis is suspected in antiphospholipid antibody syndrome, Behçet disease, and polyarteritis nodosa.
Ultrasonography with Doppler
This is used to identify thromboses in deep venous system, renal vessels, and transcranial vessels.
Positron emission tomography (PET) scan
This can detect subtle evidence of inflammation to identify potential sites of vasculitis. 
Other Tests
Other tests include the following:
- Pulmonary function tests – Both obstructive and restrictive patterns seen in pulmonary vasculitis.
- Electrocardiography – To identify signs of myocarditis or pericarditis.
- Nerve conduction studies – In patients with peripheral nerve involvement.
- Electroencephalogram – In patients with CNS involvement.
- Bronchoscopy/lavage – May be required in patients with lung involvement.
Procedures
Tissue biopsy may be necessary to confirm a diagnosis of vasculitis in systemic and cutaneous polyarteritis nodosa (PAN), ANCA vasculitis, childhood PACNS, and infrequently in Henoch-Schönlein purpura.
- Henoch-Schönlein purpura – Skin and/or renal biopsy,
- Polyarteritis nodosa – Skin biopsy,
- ANCA-vasculitides – Sinus, renal, lung, and/or skin biopsy,
- Childhood PACNS – Lesional brain biopsy often needed in small-vessel CNS vasculitis.
Histologic Findings
Histologic findings include the following:
-
Takayasu arteritis: Inflammatory infiltrate is composed of T cells. Macrophages are arranged into granulomas with giant cells. Concentric thickening of all layers of the artery wall (intima, media and adventitia) is noted.
-
Polyarteritis nodosa: Acute and segmental necrotizing vasculitis of medium-sized arteries is seen with an inflammatory infiltrate composed of neutrophils and eosinophils within the vessel walls and extravasation of erythrocytes and fibrin.
-
Churg-Strauss syndrome: In the lung, extravascular microgranulomas filled with eosinophils and intramural eosinophilic infiltrate are noted.
-
Granulomatosis with polyangiitis (GPA) (formerly Wegener granulomatosis): In the lung, granulomatous inflammation with mononuclear infiltrate including T cells, macrophages/histiocytes, and giant cells are noted.
-
GPA and microscopic polyangiitis: Renal histologic findings include “pauci-immune” (ie, little immune deposition on immunofluorescence) necrotizing glomerulonephritis with large circumferential crescents, segmental loss of basement membrane, and tubulointerstitial inflammation.
-
Henoch-Schönlein purpura: Immunofluorescence demonstrates deposition of IgA, C3, and fibrin in the walls of affected blood vessels within the dermis and the endothelial and mesangial cells of the kidney. Skin biopsy reveals features of leukocytoclastic vasculitis with infiltrate of neutrophils and mononuclear cells.
Allopathic treatment
The management of children with Kawasaki disease involves hospital admission and treatment with intravenous immunoglobulin (IVIG) and high-dose aspirin in the acute phase of the illness. Subsequently, daily low-dose aspirin is given for 6-8 weeks until follow-up echocardiography. IVIG-resistant disease may be treated with methylprednisolone and/or other immunosuppressive therapies.
Guidelines from rheumatology and the vasculitis allopathic doctors conditionally recommend the use of adjunctive glucocorticoids with IVIG as initial therapy for patients with acute Kawasaki disease who are at high risk for IVIG resistance or the development of coronary artery aneurysms.
Henoch-Schönlein purpura
The management of children with Henoch-Schönlein purpura is primarily symptomatic, and most patients do not require hospital admission. Nonsteroidal anti-inflammatory drugs (NSAIDs) can be given for joint pain or swelling. Corticosteroids may be considered in selected patients (ie, those with severe GI symptoms), but is an area of controversy in the literature. Clinically significant nephritis is typically treated with steroids and other immunosuppressive therapies.
Chronic vasculitis
Patients with chronic vasculitis should be managed by a multidisciplinary group of specialists (eg, rheumatologists, cardiologists, nephrologists) and require long-term follow-up for monitoring of relapses, disease activity, end-organ damage and morbidity associated with therapy.
Infliximab and adalimumab can be considered as first-line immunomodulatory agents for the treatment of ocular manifestations of Behçet’s disease.
Newer trails (experiments)
No allopathic therapeutic trials have looked at management of vasculitis in the pediatric population, and practice has been based on adult guidelines, which have been summarized. These recommendations provide general guidance that should be modified based on the features of each individual’s illness.
Antineutrophil cytoplasmic antibody (ANCA)-associated vasculitis
In general, adult patients with ANCA vasculitis are categorized according to different levels of severity to assist treatment decisions, as proposed by the European Vasculitis Study (EUVAS) group.
Table 1. EUVAS disease categorization of ANCA-associated vasculitis (Open Table in a new window)
| Category | Definition |
| Localized | Upper and/or lower respiratory tract disease without any other systemic
involvement or constitutional symptoms |
| Early
systemic |
Any, without organ-threatening or life-threatening disease |
| Generalized | Renal or other organ-threatening disease, serum creatinine >500
μmol/L (5.6 mg/dL) |
| Severe | Renal or other vital organ failure, serum creatinine >500 μmol/L (5.6 mg/dL) |
| Refractory | Progressive disease unresponsive to glucocorticoids and cyclophosphamide |
Experiments on induction therapy
Optimal induction therapy for patients with generalized disease (renal or other major organ involvement) is a subject of intensive study. Initial guidelines suggested a combination of cyclophosphamide and high-dose glucocorticoids. However, there have been 3 randomized controlled trials investigating the use of rituximab as an induction agent in adults with granulomatosis with polyangiitis (GPA) and microscopic polyangiitis (MPA). 
These studies have shown that rituximab is likely as effective as cyclophosphamide in inducing remission.
The most recent allopathic treatment recommendations suggest that either regimen be considered and that rituximab may be preferred when cyclophosphamide avoidance is desired (eg, due to toxicity).
Some evidence suggests that granulomatous manifestations (eg, orbital granulomas) may not respond to rituximab as well as vasculitic manifestations. With either regimen, high-dose prednisone (1 mg/kg) should be maintained for 1 month. When rapid effect is needed, intravenous (IV) pulsed methylprednisolone may be used in addition to the oral prednisone.
Van Daalen’s study
A study by van Daalen et al reported that rituximab treatment for ANCA-associated vasculitis had lower malignancy risk than in cyclophosphamide treatment and that rituximab was not associated with an increased malignancy risk compared with the general population.
Local guidelines for the prevention of glucocorticoid-induced osteoporosis should be followed in all patients. Cyclophosphamide use should be limited to 3-6 months because of potential for long-term toxicity. However, no consensus about whether pulse IV cyclophosphamide is superior to daily oral therapy. All patients who receive cyclophosphamide should also receive prophylaxis against Pneumocystis jiroveci (trimethoprim-sulfamethoxazole or pentamidine), especially those with GPA.
Mild or moderate stage
For patients with mild-to-moderate or limited disease, methotrexate can be used as a less toxic alternative for induction. However, there is some evidence that induction with methotrexate may be associated with a higher risk of relapse.
Plasma exchange is recommended as adjunctive therapy for patients with rapidly progressive severe renal disease.
Maintenance therapy
Evidence suggests that once remission is achieved with either a cyclophosphamide- or rituximab-based regimen, maintenance therapy is required to prevent relapse. One alternative is to use either methotrexate or azathioprine. A recent study has also suggested the use of biannual rituximab as maintenance therapy. The use of low-dose glucocorticoids (10 mg/d of prednisone) is also recommended.
Maintenance therapy should be continued for at least 18-24 months, and early cessation is associated with an increased risk of relapse.
Refractory or relapsing disease
The RAVE trial, a randomized, controlled, double-blinded study of cyclophosphamide versus rituximab in ANCA vasculitis, included a planned subgroup analysis of patients with refractory or relapsing disease. The findings demonstrated that rituximab was particularly effective in this population.
Several other small series also report the effectiveness of rituximab in patients with refractory or relapsing disease. Other options for refractory or relapsing disease include IVIG, mycophenolate mofetil, infliximab, 15-deoxyspergualin, and antithymocyte globulin.
Systemic polyarteritis nodosa
Patients with severe disease should receive a combination of cyclophosphamide and glucocorticoids. However, a selected group of patients with mild polyarteritis nodosa may be successfully treated with glucocorticoids alone. 
Cutaneous polyarteritis nodosa
Some patients respond to NSAIDs alone; however, most require treatment with prednisone. Steroid-sparing agents may be needed (eg, methotrexate, mycophenolate mofetil, colchicine, IVIG). Penicillin prophylaxis may prevent disease exacerbations in patients with evidence of triggering streptococcal infections.
Large vessel vasculitis
A paucity of large, controlled trials in the management of large-vessel vasculitis is noted, even in adult patients. Treatment recommendations are based on the EUVAS guidelines.
Induction therapy usually involves high-dose glucocorticoid (prednisone, 1 mg/kg/d). The initial high dose should be maintained for a month and then gradually tapered. Azathioprine or methotrexate have been used as adjuncts to steroid therapy in patients with Takayasu arteritis to improve disease control and to facilitate reduction of the steroid dose. Cyclophosphamide has been used in adults with Takayasu arteritis resistant to glucocorticoids.
In addition, tumor necrosis factor (TNF)-α inhibitors (eg, infliximab, etanercept) have been tried with encouraging results, including in a small study of 4 children.
Primary CNS vasculitis
Initiate treatment with high-dose steroids and monthly IV cyclophosphamide for 6 months, followed by maintenance with mycophenolate mofetil or azathioprine for 18 months. Anti-thrombotic therapy (heparin followed by antiplatelet) may be added for large-vessel disease.
Thrombophlebitis/hypercoagulable state
Anticoagulation is indicated for any patient with a thrombotic episode and an underlying hypercoagulable state. This usually involves initial treatment with heparin with subsequent transition to warfarin.
Refer to Antiphospholipid Antibody Syndrome for details on treatment. Generally, anticoagulant prophylaxis is not indicated in the absence of a thrombotic event. No studies in the optimal management of pediatric patients with antiphospholipid antibody syndrome have been done. The adult literature suggests that patients with documented venous or arterial thrombotic events should be managed with warfarin.
Allopathic medications
Corticosteroids
These agents have potent immunosuppressive activity with rapid onset of action. 
Used to control acute symptoms and laboratory evidence of inflammation. May decrease inflammation by reversing increased capillary permeability and suppressing PMN activity. Stabilizes lysosomal membranes and also suppresses lymphocytes and antibody production.
What is the treatment for vasculitis?
The allopathic treatment of the various forms of vasculitis is based on the severity of the illness and the organs involved.
- Treatments are generally directed toward stopping inflammation and suppressing the immune system.
- Typically, cortisone-related medications, such as prednisone, are used.
- Additionally, other immune suppression drugs, such as cyclophosphamide and others are considered.
- Additionally, affected organs (such as the heart or lungs) may require specific medical treatment when the disease is active.
The management of vasculitis is an evolving field in allopathic medicine. The allopathic programs for monitoring and treatment will continue to improve as disease patterns and causes are defined by medical research.
Immunomodulators
Class Summary
IVIG is used as first-line therapy for Kawasaki disease; it decreases risk of coronary artery aneurysms.
Immune globulin, intravenous (Sandoglobulin, Gamimune, Gamunex, Gammar-P)
Multiple mechanisms. May absorb superantigens or toxins in Kawasaki disease, saturate available Fc receptors, block cytokines, cytokine receptors, or both; absorb complement activation products, down-regulate immunoglobulin synthesis. Blocks Fc receptors on macrophages. Suppresses inducer T and B cells and augments suppressor T cells. Blocks complement cascade. May increase CSF IgG (10%).
Immunosuppressant Agents
Class Summary
These agents help control inflammatory signs and symptoms. 
Azathioprine (Imuran)
Imidazolyl derivative of 6-mercaptopurine. Antagonizes purine metabolism and inhibits synthesis of DNA, RNA, and proteins. Mechanism whereby azathioprine affects autoimmune diseases is unknown. Works primarily on T cells.
Suppresses hypersensitivities of cell-mediated type and causes variable alterations in antibody production. Immunosuppressive, delayed hypersensitivity, and cellular cytotoxicity tests are suppressed to a greater degree than antibody responses.
Works very slowly; may require 6-12 months of trial prior to effect. As many as 10% of patients may have idiosyncratic reaction disallowing use. Do not allow WBC count to drop below 3000/mL or lymphocyte count to drop below 1000/mL. Available in tablet form for PO administration or in 100-mg vials for IV injection
Cyclophosphamide (Cytoxan)
Cyclic polypeptide that suppresses some humoral activity. Chemically related to nitrogen mustards. As an alkylating agent, the mechanism of action of the active metabolites may involve cross-linking of DNA, which may interfere with growth of normal and neoplastic cells. When used in autoimmune diseases, mechanism of action is thought to involve immunosuppression due to destruction of immune cells via DNA cross-linking. In high doses, affects B cells by inhibiting clonal expansion and suppression of production of immunoglobulins. With long-term low-dose therapy, affects T-cell functions.
Methotrexate (Rheumatrex, Folex)
Antimetabolite that inhibits dihydrofolate reductase, thereby hindering DNA synthesis and cell reproduction. Effects may also be mediated by adenosine via the inhibition of aminoimidazole carboxamide ribonucleotide (AICAR) transformylase, leading to increased release of adenosine. Adjust dose gradually to attain satisfactory response.
Mycophenolate mofetil (CellCept); Mycophenolic acid (MyFortic)
Inhibits inosine monophosphate dehydrogenase and suppresses de novo purine synthesis by lymphocytes, thereby inhibiting their proliferation. Inhibits antibody production.
Tumor Necrosis Factor Inhibitor
Class Summary
Blocks the process by which activated neutrophils adhere to endothelium and stimulate lysis of endothelial cells in the presence of TNF-alpha.
Infliximab (Remicade)
Chimeric IgG1k monoclonal antibody that neutralizes cytokine TNF-alpha and inhibits its binding to TNF-alpha receptor. Reduces infiltration of inflammatory cells and TNF-alpha production in inflamed areas.
Anti-B lymphocyte agent
Class Summary
May consider these agents for conditions refractory to other treatments.
Rituximab (Rituxan)
Chimeric IgG1-kappa monoclonal antibody directed against the CD20 antigen found on the surface of normal and malignant B lymphocytes. The Fab domain binds to CD20 antigen on B lymphocytes, and the Fc domain recruits immune effector functions to mediate B-cell lysis in vitro. Possible mechanisms of cell lysis include complement-dependent cytotoxicity (CDC) and antibody-dependent cell-mediated cytotoxicity (ADCC). 
Anticoagulant
Class Summary
These agents provide immediate and long-term treatment of vascular thrombosis.
Heparin
Augments activity of antithrombin III and prevents conversion of fibrinogen to fibrin. Does not actively lyse but is able to inhibit further thrombogenesis. Prevents reaccumulation of clot after spontaneous fibrinolysis.
Provide as continuous heparin infusion to maintain aPTT at 1.5 times the control.
Enoxaparin (Lovenox)
Low molecular weight heparin. Augments activity of antithrombin III and prevents conversion of fibrinogen to fibrin. Does not actively lyse but is able to inhibit further thrombogenesis. Prevents reaccumulation of clot after spontaneous fibrinolysis.
Advantages include intermittent dosing and decreased requirement for monitoring. Heparin anti–factor Xa levels may be obtained if needed to establish adequate dosing.
Warfarin (Coumadin)
Interferes with hepatic synthesis of vitamin K–dependent coagulation factors.
Antibiotics
Class Summary
Prophylaxis for P jiroveci with cyclophosphamide therapy.
Trimethoprim-sulfamethoxazole (Bactrim, Septra)
As P jiroveci prophylaxis for patients taking cyclophosphamide. Dihydrofolate reductase inhibitor in combination with sulfonamide.
Prednisone (Deltasone, Sterapred).
Surgical Care
With involvement of the aorta and renal arteries, angioplasty and stenting of stenotic vessels has been used to improve flow (eg, in Takayasu arteritis). A significant proportion of vessels may develop restenosis, but good response to repeat procedure is noted. In addition, reconstructive surgery with graft implantation may be required.
Note that vascular procedures must be done during periods of inactive disease.
Patients with granulomatosis with polyangiitis (formerly Wegener granulomatosis) may develop subglottic stenosis; these lesions can be amenable to endoscopic management with local corticosteroid injection and/or mitomycin-C application.
Note that in granulomatosis with polyangiitis, repeated procedures are often necessary, and some patients may require tracheostomy insertion.
Homeopathic treatment for vasculitis
In Homeopathy, for the management of children with Kawasaki disease (high doses of aspirin, immunosuppressants etc.), Henoch-Schönlein purpura (nonsteroidal anti-inflammatory drugs for joint pain or swelling, corticosteroids etc.) requires not any surgery and lifelong or two-three years long therapy, no need for any antibiotics etc.
It’s very easy to treat and cure vasculitis patients with just Homeopathic medicines, no surgeries required at all, duration of treatment is no longer than 2-5 months (individual). Here are some of Homeopathic medicines for vasculitis:
Allium Sativum
Acts directly on intestinal mucous membrane increasing peristalsis. Colitis, with pathological flora. Has vaso-dilatory properties. Obese patients with dyspepsia and catarrhal affections. Hepatomegaly. Pain in hip, pain in psoas and iliac muscles. Pulmonary tuberculosis. Hemoptysis. Constant rattling of mucus in bronchi. Cough in the morning, with mucous expectoration, which is tenacious and difficult to raise. Sensitive to cold air. Dilated bronchi, with fetid expectoration. Darting pain in chest.
Pulsation in temples; catarrhal deafness. Constipation, with constant dull pains in bowels. Tongue pale, red papillae. Pain in swelling of breasts. Eruption in vagina and on breasts and vulva during menses. Diabetes. Urine increased, whitish very abundant urine, becoming cloudy from nitric acid (diabetes). Urine dark brown with copious sediment. Rheumatism. Leaping beats of the heart.
Arsenicum Album
Face swollen, pale, yellow, cachectic, sunken, cold, and covered with sweat. Tearing needle-like pains; burning. Tongue dry, clean, and red; stitching and burning pain in tongue, ulcerated with blue color. Bloody saliva. Throat swollen, edematous, constricted, burning, unable to swallow. Diphtheritic membrane dry and wrinkled. Lips black, livid. Angry, circumscribed flush of cheeks.
Palpitation, pain, dyspnea, faintness. Heart dilatation. Cyanosis. Fatty degeneration. Angina pectoris, fears suffocation. Air-passages constricted. Asthma. Hemoptysis with pain between shoulders; burning heat all over. Hemorrhoids.
Urine scanty, burning, involuntary. Albuminuria. Hematuria. Bright’s disease. Diabetes. Skin itching, burning, swellings; edema, eruption, papular, dry, rough, scaly; worse cold and scratching. Malignant pustules. Ulcers with offensive discharge. Anthrax. Poisoned wounds. Urticaria, with burning and restlessness. Psoriasis. Scirrhous. Icy coldness of body. Epithelioma of the skin. Gangrenous inflammations.
Echinacea Angustifolia
A remarkable medicine as a “corrector of blood dyscrasia”. Acute autoinfection. Blood poisoning, septic conditions. Boils. Erysipelas and foul ulcers. Gangrene. Goiter with exophthalmic symptoms. Tendency to malignancy in acute and subacute disorders. Puerperal infections. Tired feeling. Piles. Pustules. Lymphatic inflammation; crushing injuries.
Foul-smelling nasal discharges. Nostril raw, bleeding. Canker; gums recede and bleed easily; corners of mouth and lips crack; tongue dry and swollen; sores; dirty brownish. Tongue, lips, and fauces tingle, with sense of fear about heart (Acon). Tonsils purple or black, gray exudation extending to posterior nares and air-passages. Ulcerated sore throat.
Chest pain. Albuminuria, urine scanty, frequent, and involuntary. Puerperal septicemia. Aching in limbs and general lassitude. Recurring boils. Carbuncles. Lymphatics enlarged. Old tibial ulcers. Gangrene.
Calcarea Carbonica
Impaired nutrition being the keynote of its action, the glands, skin, and bones. Increased local and general perspiration, swelling of glands, scrofulous and rachitic conditions. Incipient phthisis. Tickling cough, fleeting chest pains, nausea, acidity, gets out of breath easily. Abscesses in deep muscles; polyps and exostoses. Pituitary and thyroid disfunction.
Raised blood coagulability. Great sensitiveness to cold; partial sweats. Forgetful, confused, low-spirited. Anxiety with palpitation. Obstinacy: slight mental effort produces hot head. Averse to work or exertion. Headache, with cold hands and feet. Vertigo. Scratches head on waking. 
Throbbing; cracking in ears; stitches; pulsating pain. Scrofulous inflammation with muco-purulent otorrhea and enlarged glands. Perversions of hearing; hardness of hearing. Nostrils sore, ulcerated, offensive odor in nose. Polyps. Takes cold at every change of weather. Submaxillary glands swollen. Goiter. Bleeding of gums.
Hepatomegaly. Cutting in abdomen; swollen abdomen. Incarcerated flatulence. Inguinal and mesenteric glands swollen and painful. Gall-stone colic. Increase of fat in abdomen.
Urine: dark, brown, sour, fetid, abundant, white sediment, bloody. Irritable bladder. Enuresis. Tickling cough. Extreme dyspnea. Painless hoarseness. Suffocating spells; tightness, burning and soreness, sharp pains in chest – sensitive to touch, percussion, or pressure.
Tachycardia at night, with feeling of coldness, with restless oppression of chest; after suppressed eruption. Rheumatism. Weakness of extremities. Swelling of joints, especially knee. Burning of soles of feet. Sweat of hands. Arthritic nodosities. Tearing in muscles.
Skin unhealthy; readily ulcerating; flaccid. Small wounds do not heal readily. Glands swollen. Nettle rash. Warts on face and hands. Petechial eruptions. Chilblains. Boils.
Kalium Iodatum
Infiltration and edema in fibrous and connective tissues. Glandular swellings. Purpura and hemorrhagic diathesis. Syphilis in all stages. Loss of weight, spitting of blood. Sad, anxious; harsh temper. Irritable. Violent headache. Facial neuralgia. Violent cough. Pulmonary edema. Laryngeal edema. Asthma. Dyspnea on ascending, with pain in heart. Cold travels downward to chest.
Severe bone-pains. Periosteum thickened, especially tibia, sensitive to touch. Rheumatism; worse, cold and wet. Contraction of joints. Lumbago.
Purple spots on skin; worse on legs. Acne, hydria. Small boils. Glands enlarged, indurated. Hives. Rough nodules all over. Fissured anus of infants. Tendency to edematous swellings, eyelids, mouth, uvula, etc. Acne rosacea.
Lachesis Mutus
Decomposed blood, hemorrhagic tendency. Purpura, septic states, diphtheria. Delirium tremens with trembling and confusion. Diphtheritic paralysis (Botulinum). Diphtheria carriers. Tension in various parts. Fatigue. Restless and uneasy. Pain at root of nose. Pressure and burning on vertex. Waves of pain. Headache with flickering, dim vision, pale. Defective vision after diphtheria, extrinsic muscles too weak.
Nassal bleeding, hay asthma; paroxysms of sneezing. Trifacial neuralgia. Tearing pain in jawbones. Purple, mottled, puffed; looks swollen, bloated, jaundiced, chlorotic. Gums swollen, spongy, bleed. Tongue swollen, burns, trembles, red, dry and cracked at tip, catches on teeth. Aphthous and denuded spots with burning and rawness. 
Septic parotiditis. Hepatomegaly, abdomen tympanic, sensitive, painful. Suffocation and strangulation on lying down. Cramp-like distress in precordial region. Cough; dry, suffocative fits, tickling. Breathing almost stops on falling asleep. Palpitation, with fainting spells, especially during climacteric. Constricted feeling causing palpitation, with anxiety. Cyanosis. Irregular beats.
Hot perspiration, bluish, purplish appearance. Boils, carbuncles, ulcers, with bluish, purple surroundings. Dark blisters. Bed-sores, with black edges. Blue-black swellings. Pyemia; dissecting wounds. Purpura, with intense prostration. Senile erysipelas. Wens. Cellulitis. Varicose ulcers.
Natrum Iodatum
Coryza. Hay-fever. Heart affections. Laryngitis. Pharyngitis. Rheumatism, pneumonia, asthma, chronic bronchitis, scrofula, tertiary syphilis. Hay-asthma. Chronic pharyngitis; coryza and chronic laryngitis.
Natrum Muriaticum
Dropsies and edemas, anemia and leukocytosis. Gout and rheumatic gout. Certain forms of intermittent fever, chlorosis, disturbances of the alimentary tract and skin. Great debility, weakness and weariness. Coldness. Great liability to take cold. Constrictive sensation throughout the body. Hyperthyroidism. Addison’s disease. Diabetes.
Frothy coating on tongue. Numbness, tingling of tongue, lips, and nose. Vesicles and burning on tongue. Eruptions around mouth and vesicles. Large vesicle on lips.
Bearing-down pains in women. Prolapses uteri. Shortness of breath. Tachycardia. Sensation of coldness of heart. Heart and chest feel constricted. Fluttering, palpitating; intermittent pulse. Heart’s pulsations shake body.
Pain in back. Arms, legs and knees feel weak. Skin greasy, oily. Dry eruptions. Fever blisters. Urticaria; itch and burn. Crusty eruptions. Warts. Eczema; raw, red, and inflamed. Affects hair follicles. Alopecia. Hives, itching after exertion.
Digitalis Purpura
It stimulates the heart’s muscles, increases force of systole, increases length. Pulse weak, irregular, intermittent, abnormally slow, and dropsy of external and internal parts. Weakness and dilatation of the myocardium. Slow pulse in recumbent posture, but irregular and dicrotic on sitting up. Auricular flutter and fibrillation especially when subsequent to rheumatic fever. Heart block, very slow pulse. Weakness and sinking of strength, faintness, coldness of skin, and irregular respiration; cardiac irritability; jaundice from induration and hypertrophy of the liver. Cyanotic. Cardiac muscular failure when asystole is present. Prostration from slight exertion. Collapse.
Breathing irregular, difficult. Hemoptysis with weak heart. Least movement causes violent palpitation. Frequent stitches in heart. Irregular heart especially of mitral disease. Very slow pulse. Intermits; weak. Cyanosis. Pericarditis, copious serous exudation. Dilated heart, tired, irregular. Cardiac failure following fevers. Cardiac dropsy.
Swelling of the feet. Fingers go to sleep easily. Coldness of hands and feet. Rheumatic pain in joints. Shining, white swelling of joints. Muscular debility. Nocturnal swelling of fingers. Erythema, deep red. Blue distended veins on lids, ears, lips and tongue. Dropsical. Itching and jaundiced.
Adonis Vernalis
A heart medicine, after rheumatism (rheumatic endocarditis) or influenza, or Bright’s disease. Fatty cardiac degeneration, irregular pulse, low power of contractions of heart, with polyuria. Cardiac dropsy. Low vitality, with weak heart and slow, weak pulse. Hydrothorax, ascites. Anasarca. Mitral and aortic regurgitation. Chronic aortitis, Fatty heart pericarditis. Precordial pain, palpitation, and dyspnea. Venous engorgement. Cardiac asthma. Myocarditis, irregular cardiac action, constriction and vertigo. Pulse rapid, irregular. Frequent desire to take a long breath. Feeling of weight on chest. Aching in nape. Spine stiff and aching. Edema.
Plumbum Metallicum
Hypertension and arteriosclerosis. Progressive muscular atrophy. Infantile paralysis. Locomotor ataxia. Excessive and rapid emaciation. Bulbar paralysis. Important in peripheral affections. Multiple sclerosis, posterior spinal sclerosis. Gout (Chronic).
Fear of being assassinated. Paretic dementia. Loss of memory; amnesic aphasia. Hallucinations and delusions. Intellectual apathy.
Skin yellow, dark-brown liver spots. Jaundice. Dry. Dilated veins. Paralysis of single muscles. Pains in muscles. Cramps in calves. Stinging and tearing in limbs, also twitching and tingling, numbness, pain or tremor. Feet swollen. Hands and feet cold.
Phosphorus
Vertigo. Neuralgia. Burning pains. Coldness of occiput. Face pale, sickly complexion; blue rings under eyes. Tearing pain in facial bones; circumscribed redness in one or both cheeks. Swelling and necrosis of jaw. Tongue dry, smooth, red or white, not thickly coated. Hematuria, especially in acute Bright’s disease. Aphonia. Congestion of lungs. Burning pains, heat and oppression of chest. Sharp stitches in chest; respiration quickened, oppressed. Much heat in chest.
Violent cardiac palpitation with anxiety. Pulse rapid, small, and soft. Heart dilated, especially right. Feeling of warmth in heart. Burning in back, heat between the shoulder-blades. Weak spine.
Ascending sensory and motor paralysis from ends of fingers and toes. Stitches in elbow and shoulder joints. Burning of feet. Weakness and trembling, from every exertion. Tibia inflamed and necrosed. Arms and hands become numb. Post-diphtheritic paralysis. Great drowsiness.
Wounds bleed very much, even if small; they heal and break out again. Jaundice. Little ulcer outside of large ones. Petechiae. Ecchymosis. Purpura hemorrhagic. Scurvy. Fungous hematodes and excrescences. 
Baryta Muriaticum
Arterio-sclerosis. Headaches. Vertigo, due to cerebral anemia. Tinnitus. Hypertension and vascular degeneration. Increased tension of pulse. Arterio-sclerosis with high systolic pressure, with a comparatively low diastolic tension along with cerebral and cardiac symptoms.
Indurated and narrow cardiac orifice with pain, immediately after eating, and epigastric tenderness, aneurism and chronic hypertrophy of the tonsils. Convulsions. Icy coldness of body, with paralysis. Multiple sclerosis of brain and cord. Voluntary muscular power gone but perfectly sensible. Paresis after influenza and diphtheria. General feeling of lassitude in the morning, especially weakness of the legs, with muscular stiffness.
Bronchial affection of old people with cardiac dilation. Facilitates expectoration. Arterio-sclerosis of the lung, senile asthma, arterial tension. Great increase in uric acid, diminution of chlorides.
P. S: This article is only for doctors and students having good knowledge about Homeopathy and allopathy.

For proper consultation and treatment, please visit our clinic.
 Dr. Sayyad Qaisar Ahmed (MD {Ukraine}, DHMS), Abdominal Surgeries, Oncological surgeries, Gastroenterologist, Specialist Homeopathic Medicines.
Dr. Sayyad Qaisar Ahmed (MD {Ukraine}, DHMS), Abdominal Surgeries, Oncological surgeries, Gastroenterologist, Specialist Homeopathic Medicines.
Senior research officer at Dnepropetrovsk state medical academy Ukraine.
Location: Al-Haytham clinic, Umer Farooq Chowk Risalpur Sadder (0923631023, 03119884588), K.P.K, Pakistan.
Find more about Dr Sayed Qaisar Ahmed at:
https://www.youtube.com/Dr Qaisar Ahmed