Addison disease (or Addison’s disease) is adrenocortical insufficiency due to the destruction or dysfunction of the entire adrenal cortex. It affects glucocorticoid and mineralocorticoid function. The onset of disease usually occurs when 90% or more of both adrenal cortices are dysfunctional and destroyed.
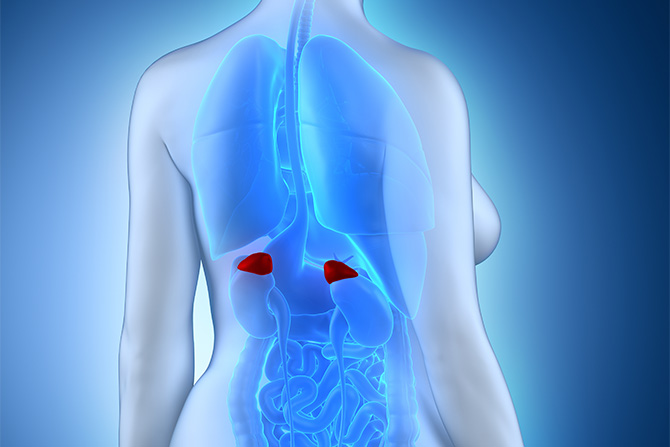
Addison’s disease affects the adrenal glands on our kidneys, the adrenal glands are responsible for hormone production.
Our adrenal glands (located on top of our kidneys) produce many of the hormones that our body needs for normal functions. Addison’s disease occurs when the adrenal cortex is damaged, and the adrenal glands don’t produce enough of the steroid hormone cortisol and aldosterone.
Cortisol regulates the body’s reaction to stressful situations. Aldosterone (ALD) helps with sodium and potassium regulation. The adrenal cortex also produces sex hormones (androgens).
Idiopathic autoimmune Addison disease tends to be more common in females and children. The most common age at presentation in adults is 30-50 years, but the disease could present earlier in patients with any of the polyglandular autoimmune syndromes or congenital adrenal hyperplasia (CAH) or in those in whom the onset is due to a disorder of long-chain fatty acid metabolism.
Signs and symptoms of Addison disease
People who have Addison’s disease may experience the following symptoms:
- Myalgias and flaccid muscle paralysis, muscle weakness,
- Fatigue and tiredness,
- Vitiligo, darkening in skin color, hyperpigmentation,
- Weight loss or decreased appetite,
- A decrease in heart rate or blood pressure,
- Low blood sugar levels,
- Weakness, fainting spells,
- Dizziness with orthostasis,
- Heightened sense of smell, taste, and hearing,
- Sores in the mouth,
- Cravings for salt,
- Nausea,
- Poor appetite,
- Vomiting,
-
Occasional diarrhea,
People living with Addison’s disease may also experience neuropsychiatric symptoms, for example:
- Irritability or depression,
- Lack of energy,
- Sleep disturbances.
Signs and symptoms of acute Addison disease:
-
Patients in acute adrenal crisis most often have prominent nausea, vomiting, and vascular collapse; they may be in shock and appear cyanotic and confused,
-
Abdominal symptoms may take on features of an acute abdomen,
-
Patients may have hyperpyrexia, with temperatures reaching 105° F or higher, and may be comatose,
-
In acute adrenal hemorrhage, the patient, usually in an acute care setting, deteriorates with sudden collapse, abdominal or flank pain, and nausea with or without hyperpyrexia.
If Addison’s disease goes untreated for too long, it can become an Addisonian crisis, also known as an adrenal crisis. An Addisonian crisis is a life-threatening medical emergency. 
Symptoms associated with an Addisonian crisis can include:
- agitation,
- delirium,
- visual and auditory hallucinations.
Classification of Addison’s disease
There are three major classifications for Addison’s disease: primary, secondary, and tertiary adrenal insufficiency.
Primary adrenal insufficiency
Primary adrenal insufficiency occurs when your adrenal glands are damaged so severely that they can no longer produce hormones. This type of Addison’s disease is most often caused when our immune system attacks your adrenal glands (autoimmune disease).
Other causes of primary adrenal insufficiency include:
- Prolonged administration of glucocorticoids (also known as steroids),
- Infections in your body,
- Cancer and abnormal growths (tumors),
- Allopathic blood thinners.
Secondary adrenal insufficiency
Secondary adrenal insufficiency occurs when the pituitary gland (located in brain) can’t produce adrenocorticotropic hormone (ACTH). ACTH tells the adrenal glands when to release hormones.
Other causes of secondary adrenal insufficiency, including:
- tumors,
- allopathic medications,
- brain trauma/injury.
Tertiary adrenal insufficiency
Tertiary adrenal insufficiency originates in the hypothalamus (near the pituitary gland). The hypothalamus normally sends corticotropin-releasing hormone (CRH) to the pituitary, stimulating it to produce ACTH. When the hypothalamus fails to produce sufficient CRH, the pituitary fails in turn to produce enough hormones to stimulate the adrenal glands.
Tertiary adrenal insufficiency is most often caused by suddenly stopping allopathic corticosteroids.
Causes
The most common cause of Addison disease is idiopathic autoimmune adrenocortical insufficiency resulting from autoimmune atrophy, fibrosis, and lymphocytic infiltration of the adrenal cortex, usually with sparing of the adrenal medulla. This accounts for more than 80% of reported cases. Idiopathic autoimmune adrenocortical atrophy and tuberculosis (TB) account for nearly 90% of cases of Addison disease.
Antibodies against the adrenal tissue are present in a significant number of these patients, and evidence of cell-mediated immunity against the adrenal gland also may be present. The steroidogenic enzyme 21-hydroxylase (21OH) is the main autoantigen, but antibodies against this enzyme are not directly involved in the tissue destruction.
Patients may have a hereditary predisposition to autoimmune Addison disease.
Idiopathic autoimmune Addison disease may occur in isolation or in association with other autoimmune phenomena (Schmidt syndrome, polyglandular autoimmune disease types 1 and 2). Other autoimmune conditions linked to Addison disease include the following: 
- Celiac disease,
- Idiopathic hypoparathyroidism,
- Mucocutaneous candidiasis,
- Type 1 diabetes mellitus,
- Hashimoto thyroiditis,
- Graves disease,
- Vitiligo,
- Alopecia areata, totalis and universalis,
- Premature ovarian or testicular failure,
- Pernicious anemia,
- Myasthenia gravis,
- Idiopathic hypophysitis,
- Chronic active hepatitis,
- Primary biliary cirrhosis.
The association of Addison disease and Hashimoto thyroiditis is known as Schmidt syndrome.
The association of Addison disease with hypoparathyroidism and mucocutaneous candidiasis is described as polyglandular autoimmune syndrome type 1. Addison disease may have an autosomal recessive mode of inheritance. It has no human leukocyte antigen (HLA) associations. Addison disease is also termed autoimmune Poly endocrinopathy-candidiasis-ectodermal dystrophy (APECED). It is caused by mutations in the autoimmune regulator gene (AIRE).
The association of Addison disease with type 1 diabetes mellitus and Hashimoto thyroiditis or Graves disease is described as polyglandular autoimmune syndrome type 2 and may be associated with HLA-B8 and DR-3.
Additional causes of chronic Addison disease:
Chronic granulomatous diseases
- TB, sarcoidosis, histoplasmosis, blastomycosis, and cryptococcosis could involve the adrenal glands.
- In the pre antibiotic era, TB was the most common cause and still may be a major consideration in areas where TB is common. It tends to involve both the adrenal cortex and the medulla; however, medullary involvement may not have any major consequences.
- TB of the adrenal glands usually is a tertiary disease due to the hematogenous spread of infection to the adrenal glands, but clinical evidence of the primary infection is not always present.
-
Hematologic malignancies
- Malignant infiltration of the adrenal cortices, as with Hodgkin and non-Hodgkin lymphoma and leukemia, may cause Addison disease.
- Hodgkin and non-Hodgkin lymphoma initially could present with adrenal gland involvement and features of adrenocortical insufficiency.
-
Metastatic malignant disease – Bilateral involvement of the adrenal glands could occur in the setting of metastatic cancer of the lung, breast, or colon or renal cell carcinoma.
Acquired immunodeficiency syndrome (AIDS)
- The adrenocortical insufficiency in patients with AIDS tends to occur late and usually in the setting of a low CD4 cell count.
- It is caused by opportunistic infections such as cytomegalovirus, Mycobacterium avium intracellular, cryptococci, or Kaposi sarcoma.
- Adrenocortical hypofunction in patients with HIV may be due to glucocorticoid resistance syndrome. These patients tend to present with features of adrenocortical insufficiency and mucocutaneous hyperpigmentation but also with increased plasma and urinary cortisol levels and a slight elevation in ACTH levels. Hyperpigmentation in patients with HIV is thought to be due to elevated alpha-interferon levels.
- Another possible cause of adrenocortical insufficiency in patients with AIDS is the use of megestrol acetate (Megace) as an appetite stimulant to stem HIV wasting disease. However, this causes secondary adrenocortical insufficiency and not Addison disease. The glucocorticoid effect of megestrol acetate suppresses pituitary ACTH production and leads to secondary adrenocortical insufficiency.
Allgrove syndrome
- Although patients with congenital adrenocortical unresponsiveness to ACTH (Allgrove syndrome) may present with features of glucocorticoid deficiency and skin hyperpigmentation, the aldosterone production and function in these patients is normal and responds appropriately to low sodium intake.
- This typically presents in childhood with failure to thrive, features of adrenocortical insufficiency, and hypoglycemia.
- Some patients may have components of alacrimia and achalasia. It is also sometimes called triple A syndrome.
Abnormalities of beta oxidation of very-long-chain fatty acids
- These patients (usually men) present with adrenocortical insufficiency and features of progressive demyelination of the CNS. It is caused by mutation in the ABCD1 gene. it is the most common cause of adrenal insufficiency in a male child less than 7 years of age.
- This is caused by the accumulation of very-long-chain fatty acids (VLCFA) in various organs, including the adrenal cortex, brain, testis, and liver.
- These disorders are X-linked recessive, with poor penetrance.
- Other symptoms include cognitive dysfunction, behavioral problems, disturbance of gait, and emotional lability.
- Two subtypes are described. The first subtype is adrenoleukodystrophy (ALD). This usually presents in childhood. Thirty percent of cases may present with adrenal insufficiency before the onset of neurologic symptoms. Other features include severe hypotonia, seizure disorder, retinitis pigmentosa, and optic atrophy. The second subtype is Adreno myeloneuropathy (AMN). This usually is mild. It tends to present in the 20- to 40-year age group with features of adrenal insufficiency and progressive CNS demyelination.

Congenital adrenal hyperplasia
- Primary adrenocortical insufficiency may occur in patients with the StAR or 20,22-desmolase enzyme deficiency, 3-beta hydroxysteroid dehydrogenase enzyme deficiency, and the severe form of the 21-hydroxylase enzyme deficiency (virilizing and salt wasting).
- Infants usually present in shock, with hypoglycemia and adrenal insufficiency.
- In 3-beta hydroxysteroid dehydrogenase enzyme deficiency, female infants appear virilized, whereas male infants may have pseudohermaphroditism from insufficient androgen activity.
- Lipoid congenital adrenal hyperplasia is a severe disorder of adrenal and gonadal steroidogenesis caused by mutations in the steroidogenic acute regulatory protein (StAR). Affected children typically present with life-threatening adrenal insufficiency in early infancy due to a failure of glucocorticoid (cortisol) and mineralocorticoid (aldosterone) biosynthesis. Male infants usually have features of pseudohermaphroditism due to an associated deficiency of gonadal steroids.
- The rapid ACTH test usually helps to establish the diagnosis. Patients with CAH respond with a marked increase in 17-OH progesterone levels, an increase in other precursors preceding the enzyme block, and a subnormal cortisol response.
Allopathic Drug-related causes
- Ketoconazole inhibits the adrenal cytochrome P450 steroidogenic enzymes.
- Aminoglutethimide blocks the early conversion of cholesterol to pregnenolone by inhibiting the 20,22-desmolase enzyme.
- Mitotane (O,P’-DDD) blocks adrenal mitochondrial steroid biosynthesis.
- Busulphan, etomidate, and trilostane inhibit or interfere with adrenal steroid biosynthesis.
- Methadone, perhaps by depleting pituitary ACTH, may cause secondary adrenocortical insufficiency in some patients.
- Immune checkpoint inhibitors (ICIs) are another, albeit infrequent, cause of primary adrenal insufficiency; the disease reportedly arises in 1-2% of patients in whom programmed death-1/programmed death-ligand 1 (PD-1/PD-L1) inhibitors or cytotoxic T-lymphocyte antigen-4 (CTLA-4) inhibitors are administered as single-agent therapy and in an estimated 4-9% of patients receiving a combination of ICIs.
Abdominal irradiation
- Addison disease could result from situations where a radiation field involves the adrenal glands.
- The lag time to onset of disease usually is 2-7 years, but the disease could occur earlier depending on the dose of the radiation.
- Hypogonadotropic Hypogonadism and DAX-1 gene mutation.
Causes of acute Addison disease:
Stress – Acute adrenal crisis precipitated by infection, trauma, surgery, emotional turmoil, or other stress factors may be the initial presentation of Addison disease in as many as 25% of cases.
-
Failure to increase steroids
- Failure to appropriately increase daily replacement steroid doses in patients with adrenocortical insufficiency in times of stress could precipitate an adrenal crisis.
- Failure to adjust the replacement steroid dose in patients on cytochrome P450 enzyme-inducing medications such as rifampin and Dilantin also could precipitate an adrenal crisis.
-
Bilateral adrenal hemorrhage
- This may be the cause of an acute adrenal crisis, and it may occur as a complication of bacterial infection with Meningococcus or Pseudomonas species, as in Waterhouse-Friderichsen syndrome.
- It also may occur as a complication of pregnancy, anticoagulant therapy with heparin or warfarin, and as a complication of coagulopathies such as antiphospholipid syndrome (APS) in patients with systemic lupus erythematosus (SLE).
- The mechanism of action of adrenal hemorrhage is not fully understood. Diagnosis usually is made in the setting of a critically ill patient on anticoagulants (or with any of the causes mentioned above) who becomes acutely hypotensive with tachycardia, nausea, vomiting, fever, and confusion or disorientation. Abdominal or flank pain with associated tenderness may develop.
- A rapid ACTH test usually should be performed in this setting, and the patient should be started on hydrocortisone without waiting for the results. When time is critical, a random cortisol should be drawn and the patient started on hydrocortisone in stress doses. An abdominal computed tomography (CT) scan often reveals bilateral adrenal gland enlargement.

-
Bilateral adrenal artery emboli and bilateral vein thrombosis
- This is a very rare cause of Addison disease but may occur in critically ill patients on heparin as a complication of heparin-induced thrombosis (HIT) or as a complication of other states that predispose to thrombosis.
- It also may occur as a complication of radiographic contrast studies involving the adrenal glands.
-
Bilateral adrenalectomy for any reason
- The surgical removal of a unilateral cortisol-producing adrenal adenoma in a patient with Cushing syndrome can cause an acute adrenal crisis from secondary adrenocortical insufficiency.
- This is due to the atrophy of the normal adrenal cortex from lack of the stimulant effect of pituitary ACTH.
Workup in Addison disease/Diagnosis
The diagnosis of adrenocortical insufficiency rests on the assessment of the functional capacity of the adrenal cortex to synthesize cortisol. This is accomplished primarily by use of the rapid adrenocorticotrophic hormone (ACTH) stimulation test (Cortrosyn, cosyntropin, or Synacthen).
A quick review of the clinical presentation, physical examination findings, and laboratory findings (when available) quickly heightens the index of suspicion and possibly leads to more appropriate tests and diagnosis. A high index of suspicion is necessary for diagnosis.
-
The diagnosis of adrenocortical insufficiency rests on the assessment of the functional capacity of the adrenal cortex to synthesize cortisol. This is accomplished primarily by use of the rapid ACTH stimulation test (Cortrosyn, cosyntropin, or Synacthen).
Performing the rapid adrenocorticotrophic hormone test.
Interpreting the rapid adrenocorticotrophic hormone test, two criteria are necessary for diagnosis: (1) an increase in the baseline cortisol value of 7 mcg/dL or more and (2) the value must rise to 20 mcg/dL or more in 30 or 60 minutes, establishing normal adrenal glucocorticoid function.
A low aldosterone value of less than 5 ng/100 mL that fails to double or increase by at least 4 ng/100 mL 30 minutes after ACTH administration denotes abnormal mineralocorticoid function of the adrenal cortex. The 30-minute aldosterone value is more sensitive than the 60-minute value because aldosterone levels actually have been shown to decrease in the 60-minute sample. The absolute 30- or 60-minute cortisol value carries more significance than the incremental value, especially in patients who may be in great stress and at their maximal adrenal output. These patients may not show a significant increase in cortisol output with ACTH stimulation. A normal 30- or 60-minute rapid ACTH test excludes Addison disease but may not adequately exclude mild impairment of the hypothalamic pituitary adrenal axis in secondary adrenal insufficiency.
In patients with Addison disease, both cortisol and aldosterone show minimal or no change in response to ACTH, even with prolonged ACTH stimulation tests lasting 24-48 hours. When the results of the rapid ACTH test are equivocal and do not meet the 2 criteria mentioned above, further testing might be required to distinguish Addison disease from secondary adrenocortical insufficiency. Plasma ACTH values and prolonged ACTH stimulation tests may be useful in making this distinction. 
Note:
1- ACTH is unstable in plasma, and specimen collection and storage may require special attention. The specimen should be collected in iced anticoagulated plastic containers and frozen immediately.
2- ACTH levels also may be high in patients recovering from steroid-induced secondary adrenocortical insufficiency and in patients with ACTH-refractory syndromes.
3- ACTH inducing tests such as metyrapone stimulation and insulin-induced hypoglycemia, which may be useful in the evaluation of some cases of secondary adrenocortical insufficiency, have no role in the diagnosis of Addison disease and may in fact be lethal to the patient with Addison disease.
4- In acute adrenal crisis, where treatment should not be delayed in order to do the tests, a blood sample for a random plasma cortisol level should be drawn prior to starting hydrocortisone replacement.
Other laboratory tests
-
Comprehensive metabolic panel
- The most prominent findings are hyponatremia, hyperkalemia, and a mild non–anion-gap metabolic acidosis due to the loss of the sodium-retaining and potassium and hydrogen ion-secreting action of aldosterone.
- Urinary and sweat sodium also may be elevated.
- The most consistent finding is elevated blood urea nitrogen (BUN) and creatinine due to the hypovolemia, a decreased glomerular filtration rate, and a decreased renal plasma flow.
- Hypercalcemia, the cause of which is not well understood, may be present in a small percentage of patients. However, hypocalcemia could occur in patients with Addison disease accompanied by idiopathic hypoparathyroidism.
- Hypoglycemia may be present in fasted patients, or it may occur spontaneously. It is caused by the increased peripheral utilization of glucose and increased insulin sensitivity. It is more prominent in children and in patients with secondary adrenocortical insufficiency.
- Liver function tests may reveal a glucocorticoid-responsive liver dysfunction.
-
CBC count
- CBC count may reveal a normocytic normochromic anemia, which, upon initial presentation, may be masked by dehydration and hemoconcentration. Relative lymphocytosis and eosinophilia may be present.
- All of these findings are responsive to glucocorticoid replacement.
-
Thyroid-stimulating hormone
- Increased thyroid-stimulating hormone (TSH), with or without low thyroxine, with or without associated thyroid autoantibodies, and with or without symptoms of hypothyroidism, may occur in patients with Addison disease and in patients with secondary adrenocortical insufficiency due to isolated ACTH deficiency. These findings may be slowly reversible with cortisol replacement. [51]
- In the setting of both adrenocortical insufficiency and hypothyroidism that requires treatment, corticosteroids should be given before thyroid hormone replacement to avoid precipitating an acute adrenal crisis.
-
Autoantibody testing
Thyroid autoantibodies, specifically antithyroglobulin (anti-Tg) and anti-microsomal or antithyroid peroxidase (anti-TPO) antibodies, and/or adrenal autoantibodies may be present.
-
Prolactin testing
- Modest hyperprolactinemia has been reported in cases of Addison disease and also in secondary adrenocortical insufficiency. It is responsive to glucocorticoid replacement.
- The cause of the hyperprolactinemia is thought to be the hyperresponsiveness of the lactotroph to thyrotropin-releasing hormone (TRH) in the absence of the steroid-induced or steroid-enhanced hypothalamic dopaminergic tone.
Imaging Studies
Chest radiograph:
-
The chest radiograph may be normal but often reveals a small heart.
-
Stigmata of earlier infection or current evidence of TB or fungal infection may be present when this is the cause of Addison disease.
ECG may show low-voltage QRS tracing with nonspecific ST-T wave changes and/or changes due to hyperkalemia. These changes are reversible with glucocorticoid replacement.
Sputum examination, examination of gastric washings for acid-fast and alcohol-fast bacilli, and a Mantoux or purified protein derivative (PPD) skin test may be needed if TB is thought to be the cause.
CT scan:
-
Abdominal CT scan may be normal but may show bilateral enlargement of the adrenal glands in patients with Addison disease because of TB, fungal infections, adrenal hemorrhage, or infiltrating diseases involving the adrenal glands.
-
In Addison disease due to TB or histoplasmosis, evidence of calcification involving both adrenal glands may be present.
-
In idiopathic autoimmune Addison disease, the adrenal glands usually are atrophic.
Allopathic treatment for Addison disease
There is no treatment in allopathy for Addison disease. The only goals of pharmacotherapy are to  reduce morbidity and to prevent complications. Corticosteroid drugs are used for replacement therapy in Addison disease and secondary adrenocortical insufficiency. Hydrocortisone sodium succinate or phosphate is the drug of choice for daily maintenance in these conditions and in the allopathic treatment of acute adrenal crisis.
reduce morbidity and to prevent complications. Corticosteroid drugs are used for replacement therapy in Addison disease and secondary adrenocortical insufficiency. Hydrocortisone sodium succinate or phosphate is the drug of choice for daily maintenance in these conditions and in the allopathic treatment of acute adrenal crisis.
In patients in acute adrenal crisis, intravenous (IV) access should be established urgently, and an infusion of isotonic sodium chloride solution should be begun to restore volume deficit and correct hypotension. Some patients may require glucose supplementation. Some patients may require glucose supplementation. The precipitating cause should be sought and corrected where possible.
In stress situations, the normal adrenal gland output of cortisol is approximately 250-300 mg in 24 hours. This amount of hydrocortisone in soluble form (hydrocortisone sodium succinate or phosphate) should be given, preferably by continuous infusion.
- Administer 100 mg of hydrocortisone in 100 cc of isotonic sodium chloride solution by continuous IV infusion at a rate of 10-12 cc/h. Infusion may be initiated with 100 mg of hydrocortisone as an IV bolus. Some hospitals mix 300-400 mg in 1 liter saline and infuse over 24 h to avoid needing to renew the infusion every 8-10 hours.
- An alternative method of hydrocortisone administration is 100 mg as an IV bolus every 6-8 hours.
- The infusion method maintains plasma cortisol levels more adequately at steady stress levels, especially in the small percentage of patients who are rapid metabolizers and who may have low plasma cortisol levels between the IV boluses.
Clinica improvement
Clinical improvement, especially blood pressure response, should be evident within 4-6 hours of hydrocortisone infusion. Otherwise, the diagnosis of adrenal insufficiency would be questionable.
After 2-3 days, the stress hydrocortisone dose should be reduced to 100-150 mg, infused over a 24-hour period, irrespective of the patient’s clinical status. This is to avoid stress gastrointestinal bleeding.
As the patient improves and as the clinical situation allows, the hydrocortisone infusion can be gradually tapered over the next 4-5 days to daily replacement doses of approximately 3 mg/h (72-75 mg over 24 h) and eventually to daily oral replacement doses, when oral intake is possible.
As long as the patient is receiving 100 mg or more of hydrocortisone in 24 hours, no mineralocorticoid replacement is necessary. The mineralocorticoid activity of hydrocortisone in this dosage is sufficient.
Thereafter, as the hydrocortisone dose is weaned further, mineralocorticoid replacement should be instituted in doses equivalent to the daily adrenal gland aldosterone output of 0.05-0.20 mg every 24 hours. The usual mineralocorticoid used for this purpose is 9-alpha-fludrocortisone, usually in doses of 0.05-0.10 mg per day or every other day.
Patients may need to be advised to increase salt intake.
Surgical Care
Parenteral steroid coverage should be used in times of major stress, trauma, or surgery and during any major procedure.
During surgical procedures, 100 mg of hydrocortisone should be given, preferably by the IM route, prior to the start of a continuous IV infusion. The IM dose of hydrocortisone assures steroid coverage in case of problems with the IV access.
-
When continuous IV infusion is not practical, an intermittent IV bolus injection every 6-8 hours may be used.
-
After the procedure, the hydrocortisone may be rapidly tapered within 24-36 hours to the usual replacement doses, or as gradually as the clinical situation dictates.
-
Mineralocorticoid replacement usually can be withheld until the patient resumes daily replacement steroids.
Corticosteroid Class Summary
These drugs are used for replacement therapy in Addison disease and secondary adrenocortical  insufficiency.
insufficiency.
Prednisone (Deltasone, Sterapred, Orasone)
Used for glucocorticoid hormone replacement. Longer acting than hydrocortisone, with a biologic half-life of 18-36 h.
Fludrocortisone (Florinef)
Synthetic adrenocortical steroid with very potent mineralocorticoid activity. For use in Addison disease and states of aldosterone deficiency.
Hydrocortisone sodium succinate or phosphate (Cortef, Hydrocortone)
Drug of choice for steroid replacement in acute adrenal crisis and for daily maintenance in patients with Addison disease or secondary adrenocortical insufficiency. Has both glucocorticoid and mineralocorticoid properties. Biologic half-life is 8-12 h. Easiest way to set up infusion is to have pharmacy mix 100 mg of hydrocortisone in 100 mL of 0.9 saline.
Further Outpatient Care
Patients on steroid replacement therapy need to be closely monitored by their primary care physician and by an endocrinologist.
Close monitoring for any signs of inadequate replacement (eg, morning headaches, weakness, and dizziness) and any signs of over-replacement (eg, cushingoid features) should prompt appropriate dosage adjustment. A periodic bone dual-energy radiographic absorptiometry scan may be useful in detecting early osteoporosis in patients who are inadvertently over-replaced with maintenance steroids.
Additional concerns (side effects of allopathic drugs) may include hypothyroidism, impotency, infertility, and bone loss.
Homeopathic treatment for Addison disease
Homeopathy has many well proven (more then 200 years in use) medicines for adrenal gland diseases like Addison disease, here are very few of them: 
Ammonium Carbonicum
Fat patients with weak heart. Pulsating forehead. Shocks through head. Burning of eyes. Photophobia. Forgetful, ill-humored. Eyestrain. Asthenopia. Hardness of hearing. Shocks through ears, eyes, and nose, when gnashing teeth, Cracking of jaw on chewing.
Tetters around mouth. Boils and pustules. Violent itching and burning blisters. Scarlet rash. Miliary rash. Malignant scarlatina. Faintly developed eruptions from defective vitality. Erysipelas in the aged, with brain symptoms. Eczema in the bends of extremities, between legs, about anus and genitals.
Tonsillitis, tendency to gangrenous ulceration of tonsils. Diphtheria. Constipation. Weeping hemorrhoids. Frequent desire to urinate, involuntary at night. Tenesmus of bladder. Urine white, sandy, bloody, copious, turbid and fetid.
Itching, swelling and burning of pudendum. Burning leucorrhea. PCOs, PCODs, Menses too frequent, profuse, early, copious, clotted, black; colicky pains, and hard, difficult stool, with fatigue, especially of thighs; yawning and chilliness. Tearing in joints pain/diseases. OA, RA, OP.
Natrum Muriaticum
Great debility: most weakness felt in the morning in bed. Coldness. Emaciation most notable in neck. Hyperthyroidism. Goiter. Addison’s disease. Diabetes. Cushing syndrome. Psychic causes of disease. Depressed, particularly in chronic diseases. Consolation aggravates. Irritable. Awkward, hasty. Wants to be alone to cry. Head throbs. Blinding headache. Chronic headache, semi-lateral, congestive, from sunrise to sunset, with pale face, nausea, vomiting; periodical; from eyestrains; menstrual. Sinus inflammation. Eyes muscles weak and stiff. Tinnitus.
Dry eruptions, especially on margin of hairy scalp and bends of joints. Fever blisters. Urticaria; itch and burn. Crusty eruptions. Warts. Eczema – raw, red, and inflamed. Alopecia. Hives, itching after exertion. Greasy skin.
Pain just after urinating. Increased, involuntary when walking, coughing, etc. Impotence with retarded emission.
Menses irregular; usually profuse. Vagina dry. Leucorrhea acrid, watery. Bearing-down pains.
Palms hot and perspiring. Arms and legs, but especially knees, feel weak. Lumbago. Numbness and tingling in fingers and lower extremities. Cracking in joints on motion. Coldness of legs with congestion to head. 
Ignatia Amara
Changeable mood; introspective; silently brooding. Melancholic, sad, tearful. Not communicative. Sighing and sobbing. Aftershocks, grief, disappointment. Head feels hollow, heavy; worse, stooping. Severe headache. Asthenopia, with spasms of lids and neuralgic pain about eyes. Flickering zig zags.
Twitching of facial muscles, and lips. Changes color when at rest. Mouth constantly full of saliva. Toothache; worse after drinking coffee and smoking. Feeling of a lump in throat. Tendency to choke, globus hystericus. Sore throat: stitches when not swallowing. Stitches between acts of swallowing. Stitches extend to ear. Tonsils inflamed, swollen, with small ulcers. Follicular tonsillitis.
Chronic constipation. Anal prolapsus. PCO, menses, black, too early, too profuse, or scanty. Excoriation, especially around vagina and mouth. Feminine sexual frigidity. Suppression from grief. Jerking of limbs. Pain in tendo-Achilles and calf. Ulcerative pain in soles.
Lycopodium Clavatum
Lycopodium is adapted more especially to ailments gradually developing, functional power weakening, with failures of the digestive powers, liver function is seriously disturbed. Atony. Malnutrition. Mild temperaments of lymphatic constitution, with catarrhal tendencies; older persons, where the skin shows yellowish spots, earthy complexion, uric acid diathesis, etc; also precocious, weakly children. kidney affections, red sand in urine, backache, in renal region; worse before urination. Deep-seated, progressive, chronic diseases. Carcinoma. Cushing syndrome. Emaciation.
Debility in morning. Marked regulating influence upon the glandular (sebaceous) secretions. Pre-senility. Ascites, in liver disease. Lycopodium patient is thin, withered, full of gas and dry. Poor immune system; has poor circulation, cold extremities. Pains come and go suddenly. Sensitive to noise and odors. Melancholy. Extremely sensitive. Averse to undertaking new things. Day and/or night-blindness. Skin infections. Eating disorders, Indigestion.
UTIs, Infertility. Erectile dysfunctions. PCO and PCODs. Sciatica, Arthritis. Osteoarthritis. Osteopenia. Osteoporosis.
Pulsatilla
Wandering stitches about head; pains extend to face and teeth; vertigo. Frontal and supraorbital pains. Neuralgic pains. Hysteria. Coldness between shoulders; Hump between shoulders. Pressure on vertex. ENT infections. Skin infections. Indigestion, eating disorders, liver diseases, gallbladder diseases, pancreatitis. Polyuria, micturition. PCOs, PCODs. Prostate cancer. Tumors anywhere in the body. Lumbago. Extremities pain – muscular and/or bones/joints. 
Graphitus
Best choice for patients with tendency to skin affections and constipation, fat, chilly, and costive, with delayed menstrual history, take cold easily. Patient impudent, teasing, laugh at reprimands. Has a particular tendency to develop the skin phase of internal disorders. Eradicates tendency to erysipelas. Anemia with redness of face. Tendency to obesity. Swollen genitals. Gushing leucorrhea. Aids absorption of cicatricial tissue. Induration of tissue. Cushing syndrome. Cancer of pylorus. Duodenal ulcer. Ophthalmic diseases. Ear infections. Skin infections. GIT infections. PCOS, leucorrhea and other uterine infections, tumors, cancers.
Alumina
A very general condition corresponding to this drug is dryness of mucous membranes and skin, and tendency to paretic muscular states. Old people, with lack of vital heat, or prematurely old, with debility. Sluggish functions, heaviness, numbness, and staggering, and the characteristic constipation find an excellent remedy in Alumina. Disposition to colds in the head, and eructation in spare, dry, thin subjects. Delicate patients, addicted to artificial/nonorganic foods.
Throbbing headaches, object seems yellow. Tinnitus. ENT infections. Skin infections. Liver weakness. Severe constipation. Extremities thin while trunk fatty. Cancers. Tumors. Prostate cancer.
Silica Tera
Neurasthenic states, and increased susceptibility to nervous stimuli and exaggerated reflexes. Diseases of bones, caries and necrosis. Fibrotic conditions and scar-tissue. Tumors. Cancers. Organic changes in an organ. Periodical states; abscesses, quinsy, headaches, spasms, epilepsy. Keloid growth. Epilepsy. Infections of ENT. Infections of skin and bones/joints. GIT infections. UTIs. PCODs and uterine infections, tumors.
Staphysagria
Nervous affections with marked irritability, diseases of the Genito-urinary tract and skin. Impetuous, violent outbursts of passion, hypochondriacal, sad. Very sensitive as to what others say about her. Dwells on sexual matters; prefers solitude. Peevish. Brain feels squeezed. Sensation of something in forehead. Tumors. ENT infections. Eating disorders. Self-abuse. Spermaturia. PCOs and uterine infection and tumors. Skin infections.
Dulcamara
Dulcamara has a specific relation also to the skin, glands, and digestive organs, mucous membranes secreting more profusely while the skin is inactive. The rheumatic troubles. One-sided spasms with speechlessness. Paralysis of single parts. Congestive headache, with neuralgia and dry nose. Constant ENT infections. Skin infections. Indigestion. UTi; Anuria, Micturition, Polyuria etc. PCOS along with skin diseases. Bones and/joints infections; Muscular weakness. 
Causticum
Manifests its action mainly in chronic rheumatic, arthritic and paralytic affections, indicated by the tearing, drawing pains in the muscular and fibrous tissues, with deformities about the joints, progressive loss of muscular strength, tendinous contractures. Broken down senile. In catarrhal affections of the air passages. Restlessness at night, with tearing pains in joints and bones, and faint-like sinking of strength. This weakness progresses until we have gradually appeared paralysis. Local paralysis, vocal cords, muscles of deglutition, of tongue, eyelids, face, bladder and extremities. Children are slow to walk. The skin is of a dirty white sallow, with warts, especially on the face. Emaciation due to disease, worry, etc, and of long standing. Burning, rawness, and soreness.
Arsenicum Album
A profoundly acting remedy on every organ and tissue. Debility, exhaustion, and restlessness, irritable weakness. Burning pains, burning headaches. Anemia and chlorosis. Degenerative changes. Gradual loss of weight. Septic infections and low vitality. Skin infections, skin ulcers. UT infections. Joints and bone diseases. ENT infections. GIT infections. UTI and analyzation. Extremities. Trembling, twitching, spasms, weakness, heaviness, uneasiness. Cramps in calves. Swelling of feet. Sciatica. Burning pains. Peripheral neuritis. Diabetic gangrene. Paralysis of lower limbs with atrophy.
Carbo Animalis
Seems to be especially adapted to scrofulous and venous constitutions, old people, and after debilitating disease, with feeble circulation and lowered vitality. Glands are indurated, veins distended, skin blue. Stitch remaining after pleurisy. Easily strained from lifting. Weakness of nursing women. Ulceration and decomposition. All its secretions are offensive. Causes local congestions without heat. Brain tumors. Severe headaches. Weak digestion. PCOs and tumors. Skin infections. Joints pain, weakness. Coccyx pain and burning. Fatty liver. Paralysis of interosseous muscles of feet and hands.
Ferrum Picricum
Warts and epithelial growths; corns with yellowish discoloration. Senile hypertrophy of the prostate. Epistaxis. Chronic deafness and tinnitus due to gout. Meatus dry. Locomotor ataxia. Pseudo leukemia. ENT infection. Joints weakness, joints pains. Urinary tract infections.
Natrum Sulphuricum
Melancholy, with periodical attacks of mania. Suicidal tendency. Occipital pain. Piercing stitches in ears. Vertigo; relieved by sweat on head. Bursting feeling on coughing. Hot feeling on top of head. ENT infection. Photophobia. Gallbladder infection. Diabetes. Herpetic uvulitis. Leucorrhea and other uterine infections and tumors. Lumbago. Bones and joints pains, infections.
Natrum Carbonicum
All the Natrum stimulate cellular activity and increase oxidation and metabolism. Severe headaches. ENT infections. Skin infections, freckles. GIT – eating disorders. Uterine weakness, tumors and infections. Old sprains. Severe weakness of limbs. Easy dislocation and spraining of ankles. Joints diseases and infections. 31680-9/asset/1999a4d4-c70a-4cab-a68e-e44cc83e16eb/main.assets/gr1_lrg.jpg)
Plumbum Metallicum
Mental depression. Fear of being assassinated. Quiet melancholy. Slow perception; loss of memory; amnesic aphasia. Hallucinations and delusions. Intellectual apathy. Memory impaired. Paretic dementia. Weakness or loss of memory. Slow of perception; increasing apathy. Unable to find proper word while talking. Coma. Imbecility. Dementia. Mania. Delirium; alternating with colic. Fury. Frantic delirium (bites, strikes).
Head: Delirium alternating with colic. Pain as if a ball rose from throat to brain. Heaviness of head. Hair very dry. Tinnitus. Dizziness to the extent of failing senseless. Tearing in forehead and temples. Lancinating headache. Congestion of blood to head, with pulsation and heat. Violent pains in integuments of skull from occiput to forehead. Occasional sudden diminution of hearing. Loss of smell.
Bloated Ness of face. Semi lateral swelling of face. Paralysis of lower two branches of facial nerve. Hippocratic face. Boring in lower jaw. Exfoliation (painless) of lips. Cramps in jaw. Lockjaw.
Eyes: Pupils contracted. Yellow. Optic nerve inflamed. Intraocular, suppurative inflammation. Paralysis of upper eyelids. Glaucoma, especially if secondary to spinal lesion. Optic neuritis, central scotoma. Sudden loss of sight after fainting. Hypopyon. Myopia. Diplopia. Blindness, as from amaurosis. Optic neuritis.
Convulsive movements of arms and hands. Weakness and painful paralysis of arms and hands. Painful sensation of paralysis in lower extremities. Numbness of legs and feet
Carboneum Sulphuratum
Hallucinations. Headache and dizziness. Noises in head. Senselessness of lips/tongue etc. Optic neuritis. Vision greatly impaired. Color-blindness. Hearing impaired. Tinnitus atrium. Meniere’s disease. Numbness of arms and hands.
Baryta Carbonica
Loss of memory, mental weakness. Irresolute. Vertigo; stitches, when standing in the sun, extending through head. Brain feels as if loose. Hair falls out. Confusion. Wens.
Alternate dilatation and contraction of pupils. Photophobia. Gauze before eyes. Cataracts. Pressure in brain under vertex, towards occiput. with stiffness of neck. Digging in the head, with a sensation of looseness of the brain. Numbness in skin of forehead to root of nose. Aching and burning pain in the eyes. Specks flying about, and black spots before the eyes. Sparks before the eyes in the dark. Dazzling of the eyes by the light.
Ears: Hardness of hearing. Crackling noise. Nocturnal pulsation in the ears. Glands around ears painful and swollen. Reverberation on blowing nose. Tinkling and roaring in the ears. Cracking in the ears on swallowing, on sneezing, and on walking quickly. Tearing in bone in front of ear.
Trembling of the hand when writing. Tension in the legs, as if the tendons were too short. Inquietude and trembling in the legs and feet, with paralytic weakness, or tension, as if from contraction of the tendons, in different parts. Paralysis and palsy of aged persons. Shakings and starlings of some of the limbs, and of the whole body.
Thuja Occidentalis
Acts on skin, blood, gastrointestinal tract, kidneys, and brain. Its relation to the production of pathological vegetations condylomas, warty excrescences, spongy tumors is very important. Moist mucous tubercles. Bleeding fungus growths. Naevus. Excess of vinosity. Headache as if pierced by a nail. Ciliary neuralgia. Tarsal tumors. Limbs feel as if made of wood or glass. Muscular twitching, weakness and trembling. 
Hydrastis
Cancer. Chancroids. Headache. Severe frontal headache. Taste, disordered. Throat, deafness. Throat, sore. Tongue affections.
Calcarea Carbonicum
Headache, with cold hands and feet. Icy coldness in and on the head. Epilepsy. Hydrocephalus. Hypochondriasis. Paralysis. Attacks of semi-lateral headache, with risings and nausea. Sudden attacks of paralytic weakness in the arms. Tingling in the fingers, as when they are asleep. Frequent paralytic weakness in the fingers. Heavy movement of the fingers. Contraction of the fingers. Panaras. Cramps and contractions of the limbs.
Argentum Nitricum
Addison’s disease. Cushing syndrome. Anemia. Chancre. Dyspepsia. Epilepsy. Locomotor ataxy. Neuralgia. Ophthalmia neonatorum. Paralysis. Prostate enlargement. Dullness, mental confusion, dizziness, tendency to fall sideways. Momentarily blind with mental confusion; buzzing in ears, nausea, trembling. Digging up, incisive motion, through the l. hemisphere of the brain. Pressing boring pains, in small spots; in bones. Hemicrania; epileptiform; periodic; boring pain. Paralytic heaviness and debility.
Cicuta Virosa
Cancer. Catalepsy. Cerebro-spinal meningitis. Coccygodynia. Concussions. Convulsions. Eczema. Epilepsy. Paralysis. Dementia. Giddiness and absence of mind. Giddiness with falling. Pupils either much contracted or dilated. Suspension of the sight. The objects appear double and black. Stratings and convulsive movements (involuntary) in the arms and in the fingers. Deadness of the fingers. Attacks of catalepsy, with relaxation of all the muscles, and absence of respiration. Tetanus.
Belladonna
Belladonna acts upon every part of the nervous system. Vertigo with falling. Palpitation reverberating in head with labored breathing. Convulsive motion of muscles of face. Photophobia; shooting in eyes. Exophthalmos. Ocular illusions; fiery appearance. Diplopia, vanishing of sight and great debility.
Conium Maculatum
Headache, stupefying, with nausea and vomiting. Photophobia. Paralysis of ocular muscles. Cushing syndrome. Crawling/tingling in the arms and in the hands. Extremities are heavy, weary, paralyzed; trembling; bands unsteady; fingers and toes numb. Muscular weakness, especially of lower extremities. Perspiration of hands. Putting feet on chair relieves pain.
Kalium Iodatum
Violent headache. Brain feels enlarged. Hard nodes, with severe pain. Facial neuralgia. Lancinating pain in upper jaw.
Arsenicum Bromatum
Glandular tumors and indurations, carcinoma, locomotor ataxia.
Hydrastis Canadensis
Cancer. Chancroids. Dull, heavy frontal headache over eyes. Profuse secretion of tears; smarting and burning of eyes and lids. Roaring in the ears like machinery. Otorrhea, thick mucus discharge (fetid). Partial stoppage of Eustachian tube. Throat deafness. Muscles greatly weakened. Scrofulous and cancerous cachexia. Cushing syndrome. Cancers hard, adherent, skin mottled, puckered, cutting like knives in mammae. 
Iodum
Appetite, disordered. Atrophy. Brain, atrophy of. Breasts, affections of. Cancer. Chilblains. Chyluria. Constipation. Consumption. Coryza. Cough. Croup. Debility. Diabetes. Diarrhea. Diphtheria. Emaciation. Enteric fever. Galactorrhea. Goiter Hemorrhoids. Headaches. dizziness. Cushing syndrome. Vertigo; throbbing in the head and all over the body. Vertigo with red face, palpitation, hysteria, nervousness. Headache, in hot air. Pain, as from a bruise, in the brain, with want of strength in the body, as from paralysis. Acute pressive pains in the forehead. Headache, as if a tape or band were tightly drawn around the head.
Watery white swelling of the eyelids. Dirty yellowish color of the sclerotic. Protrusion of the balls. Lachrymation. Convulsive movements and quivering of the eyes; of the (lower) eyelids. Weak sight. Dimness of vision. Diplopia. Sparks and scintillations before the eyes.
Buzzing in the ears. Hardness of hearing. Sensibility to noise.
Cadmium Sulphuratum
Corneal opacity. Eyes, affections of. Facial paralysis. Indigestion. Meningitis. Nasal polypus. Constriction; stitches; pulsation. Hammering in the head, preceding vomiting. Headache with restlessness, icy coldness of body, epistaxis, constriction in throat, thirst, nausea, vomiting. Cushing syndrome.
Night-blindness. Scrofulous inflammation. Opacity of cornea. Hot tears. Swellings of lids. Hollow eyes; blue circles.
Sounds echo in head. Nose ulcerative or cancerous smell (ozaena). Spasmodic movements of upper lip. Facial paralysis from cold air-crawling sensation-chronic eruption on forehead, nose, and round mouth. Swelling of lips.
Mortality/Morbidity
Morbidity and mortality associated with Addison disease usually are due to failure or delay in making the diagnosis or a failure to institute adequate glucocorticoid and mineralocorticoid replacement. With slow-onset chronic Addison disease, significant low-level, nonspecific, but debilitating, symptomatology may occur.
With allopathic treatment, the risk of death is more than 2-fold higher, higher than treated Homeopathically. Cardiovascular, malignant, and infectious diseases are responsible for the higher mortality rate.
P. S: This article is only for doctors having good knowledge about Homeopathy and allopathy, for learning purpose(s).
For proper consultation and treatment, please visit our clinic.
None of above-mentioned medicine(s) is/are the full/complete treatment but just hints for treatment; every patient has his/her own constitutional medicine.
 Dr. Sayyad Qaisar Ahmed (MD {Ukraine}, DHMS), Abdominal Surgeries, Oncological surgeries, Gastroenterologist, Specialist Homeopathic Medicines.
Dr. Sayyad Qaisar Ahmed (MD {Ukraine}, DHMS), Abdominal Surgeries, Oncological surgeries, Gastroenterologist, Specialist Homeopathic Medicines.
Senior research officer at Dnepropetrovsk state medical academy Ukraine.
Location: Al-Haytham clinic, Umer Farooq Chowk Risalpur Sadder (0923631023, 03119884588), K.P.K, Pakistan.
Find more about Dr Sayed Qaisar Ahmed at:
https://www.youtube.com/Dr Qaisar Ahmed
7 days back I am suffering from Urine Infection. My Father suggested me this link. Awesome blog. Followed by the above remedies now I am feeling much better then before.
3 weeks back I am having muscle pain in my abdominal area. Thanks to admin followed by the above Guidelines now I am cured. Keep sharing such good Articles. This blog is very helpful.
I am a Cricket player. 7 days back I am having mucle pain in my legs. Thanks to admin followed by these Guidelines now I am feeling better. Keep Sharing such good informative articles.
This really answered my drawback, thank you!
🥰🌹
Hi my friend! I wish to say that this article is amazing, great written and include almost all significant infos. I would like to look more posts like this.
Hello there, I discovered your web site by way of Google even as searching for a related subject, your web site came up, it seems to be good. I have bookmarked it in my google bookmarks.
Good web site! I truly love how it is simple on my eyes and the data are well written. I am wondering how I might be notified when a new post has been made. I have subscribed to your RSS which must do the trick! Have a great day!
Good day I am so excited I found your blog page, I really found you by error, while I was looking on Askjeeve for something else, Regardless I am here now and would just like to say thanks a lot for a incredible post and a all round interesting blog (I also love the theme/design), I don抰 have time to read it all at the minute but I have saved it and also added your RSS feeds, so when I have time I will be back to read much more, Please do keep up the excellent work.
Sweet blog! I found it while surfing around on Yahoo News. Do you have any suggestions on how to get listed in Yahoo News? I’ve been trying for a while but I never seem to get there! Thanks