Gallbladder stones or cholelithiasis and Urinary Tract Stones (Ureterolithiasis) are very common disorders. The majority of people with gallstones have no signs or symptoms and are unaware of their gallstones. Once symptoms develop, they are likely to continue and often will worsen.
Gallbladder stones or cholelithiasis usually form in the gallbladder; however, they also may form anywhere there is bile – in the intrahepatic, hepatic, common bile, and cystic ducts.
Gallbladder stones or cholelithiasis also may move about in the bile, for example, from the gallbladder into the cystic or the common duct.
The common types of gallbladder stones or Cholelithiasis are cholesterol, black pigment, and brown pigment.
The pain from biliary colic is a very specific type that comes on suddenly or rapidly and builds to a peak over a few minutes; however, the pain may vary in severity. The movement does not make the pain worse.
Gallbladder Stones or Cholelithiasis
Liver cells secrete the bile into small canals within the liver referred to as canaliculi. The bile flows through the canaliculi and into larger collecting ducts within the liver referred to as intrahepatic bile ducts. The bile then flows through merged intrahepatic bile ducts out of the liver as extrahepatic (outside the liver) bile ducts, (first into the two hepatic bile ducts, then into the single common hepatic duct, and finally, after the common hepatic duct is joined by the cystic duct coming from the gallbladder, into the common bile duct.
From the bile duct, bile can flow from two different directions. The first direction is through the common bile duct and directly into the intestine where the bile mixes with food and promotes digestion of food. At the same time, toxic substances that are removed by the liver from the blood are eliminated into the intestine.
The second direction is into an offshoot of the common bile duct, the cystic duct, and from there into the gallbladder. Once in the gallbladder, bile is concentrated by the removal (absorption) of water. During a meal, the muscle that makes up the wall of the gallbladder contracts and squeezes the concentrated bile in the gallbladder back through the cystic duct into the common bile duct and then into the intestine. (Concentrated bile is much more effective for digestion than the un-concentrated bile that goes from the liver straight into the intestine.) The timing of gallbladder contraction – during a meal – allows the concentrated bile from the gallbladder to mix with food.
Cholesterol gallstones
Cholesterol gallstones are primarily made up of cholesterol. They are the most common type of gallstone, comprising 80% of gallstones in individuals. Cholesterol is one of the substances (chemicals) that liver cells secrete into bile. Secretion of cholesterol into bile is an important mechanism by which the liver eliminates excess cholesterol from the body.
In order for bile to carry cholesterol, the cholesterol must be dissolved in the bile. Cholesterol is fat, however, and bile is an aqueous or watery solution; fats do not dissolve in watery solutions. In order to make the cholesterol dissolve in bile, the liver also secretes two detergents, bile acids, and lecithin, into the bile. These detergents, just like dishwashing detergents, dissolve the fatty cholesterol so that it can be carried by bile through the ducts.
If the liver secretes too much cholesterol for the number of bile acids and lecithin it secretes, some of the cholesterol does not stay dissolved. Similarly, if the liver does not secrete enough bile acids and lecithin, some of the cholesterol does not stay dissolved. In either case, the undissolved cholesterol sticks together and forms particles of cholesterol that grow in size and eventually become gallstones.
Two other processes promote the formation of cholesterol gallstones though neither process is able to cause cholesterol gallstones to form.
- The first is an abnormally rapid formation and growth of cholesterol particles into gallstones. Thus, with the same concentrations of cholesterol, bile acids, and lecithin in the bile, patients with gallstones form particles of cholesterol more rapidly than individuals without gallstones.
- The second process that promotes the formation and growth of gallstones is reduced contraction and emptying of the gallbladder that allows bile to stay in the gallbladder longer than normal so that there is more time for cholesterol particles to form and grow into gallstones.
Pigment and allopathic antibiotic caused gallstones
Pigment gallstones
Pigment gallstones are the second most common type of gallstone. Although pigment gallstones comprise only 15% of gallstones in individuals.
There are two types of pigment gallstones:
1) black pigment gallstones.
2) brown pigment gallstones.
The pigment is a waste product formed from hemoglobin (the oxygen-carrying chemical in red blood cells). The hemoglobin from old red blood cells that are being destroyed is changed into a chemical called bilirubin and released into the blood. Bilirubin is removed from the blood by the liver. The liver modifies the bilirubin and secretes the modified bilirubin into bile so that it can be eliminated from the body.
Black pigment gallstones
If there is too much bilirubin in the bile, the bilirubin combines with other constituents in bile, for example, calcium, to form pigment (so-called because it is dark brown in color). Pigment dissolves poorly in bile and, like cholesterol, it sticks together and forms particles that grow in size and eventually become gallstones. The pigment gallstones that form in this manner are called black pigment gallstones because they are black and hard.
Brown pigment gallstones
If there is a reduced contraction of the gallbladder or obstruction to the flow of bile through the ducts, bacteria may ascend from the duodenum into the bile ducts and gallbladder. The bacteria alter the bilirubin in the ducts and gallbladder, and the altered bilirubin then combines with calcium to form pigment. The pigment then combines with fats in bile (cholesterol and fatty acids from lecithin) to form particles that grow into gallstones. This type of gallstone is called a brown pigment gallstone because it is more brown than black. It also is softer than black pigment gallstones.
Other types of gallstones
Other types of gallstones are rare. Perhaps the most interesting type is the gallstone that forms in patients taking the antibiotics, especially ceftriaxone. Ceftriaxone is unusual in that it is eliminated from the body in bile in high concentrations. It combines with calcium in bile and becomes insoluble. Like cholesterol and pigment, the insoluble ceftriaxone and calcium form particles that grow into gallstones. Fortunately, most of these gallstones disappear once the antibiotic is discontinued; however, they still may cause problems until they disappear. Another rare type of gallstone is formed from calcium carbonate.
Symptom of Gallbladder stones or cholelithiasis
Biliary colic is a very specific type of pain, occurring as the primary or only symptom in 80% of people with gallstones who develop symptoms. Biliary colic occurs when the bile ducts (cystic, hepatic ducts, or common bile ducts) are suddenly blocked by a gallstone. Slowly progressing obstruction, as from a tumor, does not cause biliary colic. Behind the obstruction, fluid accumulates and distends the ducts and gallbladder.
In the case of hepatic duct or common bile duct obstruction, this is due to continued secretion of bile by the liver. In the case of cystic duct obstruction, the wall of the gallbladder secretes fluid into the gallbladder. The distention of the ducts or gallbladder causes biliary colic.
Biliary colic is a recurring symptom. Once the first episode occurs, there are likely to be other episodes. Moreover, there is a pattern of recurrence for each individual, that is, in some individuals, the episodes tend to remain frequent while in others they are infrequent.
The majority of people who develop biliary colic do not go on to develop cholecystitis or other complications. There is a misconception that contraction of the gallbladder is what causes the obstruction of the ducts and biliary colic. Eating, even fatty foods, does not cause biliary colic; most episodes of biliary colic occur during the night, long after the gallbladder has emptied.
Diagnosis
Gallbladder stones or cholelithiasis are diagnosed in one of two situations.
- When some symptoms or signs suggest the presence of gallstones and the diagnosis of gallstones is being pursued.
- Coincidentally while a non-gallstone-related medical problem is being evaluated.
Ultrasonography (US) is the most important means of diagnosing gallstones. Standard computerized tomography (CT or CAT scan) and magnetic resonance imaging (MRI) may occasionally demonstrate gallstones; however, they are not as useful compared to ultrasonography because they miss gallstones.
Two types of ultrasonographic techniques can be used for diagnosing gallstones: transabdominal ultrasonography and endoscopic ultrasonography.
Transabdominal ultrasonography
For transabdominal ultrasonography, the transducer is placed directly on the skin of the abdomen. The sound waves travel through the skin and then into the abdominal organs. Transabdominal ultrasonography is painless, inexpensive, and without risk to the patient. In addition to identifying 97% of gallstones in the gallbladder, abdominal ultrasonography can identify many other abnormalities related to gallstones. It can identify:
- A thickened wall of the gallbladder when there are cholecystitis and inflammation has thickened the wall.
- Enlarged gallbladder and bile duct due to obstruction by gallstones.
- Pancreatitis.
- Fluid surrounding the gallbladder (a possible sign of inflammation) sludge.
Transabdominal ultrasonography also may identify diseases not related to gallstones that may be the cause of the patient’s problem, for example, appendicitis. The limitations of transabdominal ultrasonography are that it can only identify gallstones larger than 4-5 millimeters in size, and it is poor at identifying gallstones in the bile ducts.
Endoscopic ultrasonography (EUS)
For endoscopic ultrasonography, a long flexible tube – the endoscope – is swallowed by the patient after he or she has been sedated with intravenous medication. The tip of the endoscope is fitted with an ultrasound transducer. The transducer is advanced into the duodenum where ultrasonographic images are obtained.
Endoscopic ultrasonography can identify gallstones and the same abnormalities as transabdominal ultrasonography; however, since the transducer is much closer to the structures of interest – the gallbladder, bile ducts, and pancreas – better images are obtained than with transabdominal ultrasonography. Thus, it is possible to visualize smaller gallstones with EUS than transabdominal ultrasonography. EUS also is better at identifying gallstones in the common bile duct.
Although endoscopic ultrasonography is in many ways better than transabdominal ultrasonography, it is expensive, not available everywhere, and carries a small risk of complications such as those associated with the use of intravenous sedation, and intestinal perforation by the endoscope. Fortunately, transabdominal ultrasonography usually gives most of the necessary information, and endoscopic ultrasonography is needed only infrequently. Endoscopic ultrasonography also is a better way than transabdominal ultrasonography to evaluate the pancreas for pancreatitis or its complications.
Magnetic resonance cholangiopancreatography (MRCP)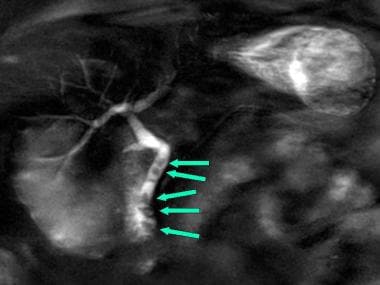
Magnetic resonance cholangiopancreatography or MRCP is a modification of magnetic resonance imaging (MRI) that allows the bile and pancreatic ducts to be examined.
- For MRCP, the patient is placed in a strong magnetic field that through its energy-carrying radio waves aligns (magnetizes) the protons in the molecules of water in the tissues. (Protons are parts of the atoms that make up water molecules. All tissues in the body contain water though they contain different amounts of water.)
- Energy-carrying radio waves are passed through the tissues, and the energy is absorbed by the water’s protons.
- The radio waves are turned off, and the protons release the energy they had absorbed.
- The released energy is used to form an image of the tissues and organs of the body.
- The MRI separates tissues and organs based on their concentration of water. Since different tissues contain different amounts of water, MRCP is very good at providing images of organs and tissues.
- Since bile is mostly water, MRCP gives an excellent image of bile within the gallbladder and bile ducts. The pancreatic duct, which, like the bile ducts, is filled with a watery fluid, also is seen well.
- Often an intravenous injection of a dye is used to better delineate the bile and pancreatic ducts.
The procedure is called cholangitis (referring to the bile ducts) pancreatography (referring to the pancreatic duct) because it can demonstrate the bile and pancreatic ducts.
MRCP has in many instances replaced other procedures such as Chole scintigraphy (HIDA scan) and endoscopic retrograde cholangiopancreatography (ERCP) for evaluating the bile ducts. It can identify gallstones in the bile ducts, obstruction of the ducts, and leaks of bile. There are no risks to the patient with MRCP except for very rare reactions to the injected dye.
Cholescintigraphy (HIDA scan)
Chole scintigraphy is a procedure done by nuclear medicine physicians. It also is referred to as a HIDA scan or a gallbladder scan.
- For a HIDA scan, a radioactive chemical is injected intravenously into a patient.
- The radioactive chemical is removed from the blood by the liver and secreted into the bile.
- The chemical then disperses everywhere that the bile goes-into the bile ducts, the gallbladder, the intestine, and anyplace else that bile goes.
- A camera that senses radioactivity (like a Geiger counter) is then placed over the patient’s abdomen and a “picture” of the liver, bile ducts, and gallbladder is obtained which corresponds to where the radioactive chemical has traveled within, or outside of the bile-filled bile ducts, and gallbladder.
HIDA scans are used to identify obstruction of the bile ducts, for example, by a gallstone. They also may identify bile leaks and fistulas. There are no risks to the patient with HIDA scans.
Chole scintigraphy also is used to study the emptying of the gallbladder. Some patients with gallstones have had gallbladder inflammation due to recognized or unrecognized episodes of cholecystitis. (There also are uncommon, non-gallstone-related causes of inflammation of the gallbladder.) The inflammation can result in scarring of the gallbladder’s wall and muscle, which reduces the ability of the gallbladder to contract. As a result, the gallbladder does not empty normally. During Chole scintigraphy, a synthetic hormone related to cholecystokinin (the hormone the body produces and releases during a meal to cause the gallbladder to contract) can be injected intravenously to cause the gallbladder to contract and squeeze out its bile and radioactivity into the intestine. If the gallbladder does not empty the bile and radioactivity normally, it is assumed that the gallbladder is diseased due to gallstones or non-gallstone-related inflammation.
The problem with interpreting a gallbladder emptying study is that many people with normal gallbladders have abnormal emptying of the gallbladder. Therefore, it is hazardous to base a diagnosis of a diseased gallbladder on abnormal gallbladder emptying alone.
Endoscopic retrograde cholangiopancreatography (ERCP)
ERCP is a combined endoscope and X-ray procedure performed to examine the duodenum (the first portion of the small intestine), the papilla of Vater (a small nipple-like structure where the common bile and pancreatic ducts enter the duodenum), the gallbladder, and bile and pancreatic ducts.
The procedure is performed by using a long, flexible, side-viewing instrument (a duodenoscope, a type of endoscope) about the diameter of a fountain pen. The duodenoscope is flexible and can be directed and moved around the many bends of the stomach and intestine. The video-endoscope is the most common type of duodenoscope and uses a chip at the tip of the instrument to transmit video images to a TV screen.
- First, the patient is sedated with intravenous drugs.
- The duodenoscope is inserted through the mouth, to the back of the throat, down the food pipe (esophagus), through the stomach, and into the first portion of the small intestine (duodenum).
- Once the papilla of Vater is identified, a small plastic catheter (cannula) is passed through a channel in the duodenoscope into the papilla of Vater, and into the bile ducts and the pancreatic duct.
- Contrast material (dye) is injected, and x-rays are taken of the bile ducts, gallbladder, and/or the pancreatic duct.
ERCP can identify; 1) gallstones in the gallbladder (though it is not particularly good at this) and 2) blockage of the bile ducts, for example, by gallstones, and 3) bile leaks. ERCP also may identify diseases not related to gallstones that may be the cause of the patient’s problem, for example, pancreatitis or pancreatic cancer.
An important advantage of ERCP is that instruments can be passed through the same channel as the cannula used to inject the dye to extract gallstones stuck in the common and hepatic ducts. This can save the patient from having an operation. ERCP has several risks associated with it, including the drugs used for sedation, perforation of the duodenum by the duodenoscope, and pancreatitis (due to damage to the pancreas). If gallstones are extracted, bleeding also may occur as a complication.
Liver and pancreatic blood tests
When the liver or pancreas becomes inflamed or their ducts become obstructed and enlarged, the cells of the liver and pancreas release some of their enzymes into the blood. The most commonly measured liver enzymes in blood are aspartate aminotransferase (AST) and alanine aminotransferase (ALT). The most commonly measured pancreatic enzymes in blood are amylase and lipase. Many medical conditions that affect the liver or pancreas cause these blood tests to become abnormal, so these abnormalities alone cannot be used to diagnose gallstones. Nevertheless, abnormalities of these tests suggest there is a problem with the liver, bile ducts, or pancreas, and gallstones are a common cause of such abnormal tests, particularly during sudden obstruction of the bile ducts or pancreatic ducts. Thus, abnormal liver and pancreatic blood test direct attention to the possibility that gallstones may be causing the acute problem.
Duodenal biliary drainage
Duodenal biliary drainage is a procedure that occasionally can be useful in diagnosing gallstones; however, it is not often used. As previously discussed, gallstones begin as microscopic particles of cholesterol or pigment that grow in size. It is clear that some people who develop biliary colic, cholecystitis, or pancreatitis have only these particles in their gallbladders, yet the particles are too small to obstruct the ducts. There are two potential explanations for how obstruction might occur in this situation. The first is that a small gallstone initially caused an obstruction before passing through the bile ducts into the intestine. The second is that particles passing through the bile ducts can “irritate” the ducts, causing spasm of the muscle within the walls of the ducts (which obstructs the flow of bile) or inflammation of the duct that causes the wall of the duct to swell (which also obstructs the duct).
- For duodenal drainage, a thin plastic or rubber tube with several holes at its tip is passed through a patient’s anesthetized nostril, down the back of the throat, through the esophagus and stomach, and into the duodenum where the bile and pancreatic ducts enter the small intestine. This is done with the help of an x-ray (fluoroscopy).
- Once the tube is in place, a synthetic hormone related to cholecystokinin, the hormone that is normally released after a meal to cause the gallbladder, is injected intravenously. As a result, the gallbladder contracts and squeezes out its concentrated bile into the duodenum.
- The bile is sucked through the tube in the duodenum and examined for the presence of small cholesterol and pigment particles under a microscope.
The risks to the patient of duodenal drainage are minimal. (There have been no reports of reactions to the synthetic hormone.) Nevertheless, duodenal drainage is uncomfortable.
A modification of duodenal drainage involves the collection of bile through an endoscope at the time of an upper gastrointestinal endoscopy-either esophagogastroduodenoscopy (EGD) or ERCP.
Oral cholecystogram (OCG)
The oral Chole cystogram or OCG is a radiologic (X-ray) procedure for diagnosing gallstones.
- The patient takes iodine-containing tablets for one or two nights in a row and then has an X-ray of the abdomen.
- The iodine is absorbed from the intestine into the blood, removed from the blood by the liver, and excreted into the bile.
- In the gallbladder, the iodine becomes concentrated along with the bile.
- On the X-ray, the iodine, which is dense and stops X-rays, fills the gallbladder and outlines the gallstones that are not dense, and allows X-rays to pass through them. The ducts cannot be seen on the x-ray because the iodine is not concentrated in the ducts.
The OCG is an excellent procedure for diagnosing gallstones; it finds 95% of them. The OCG has been replaced, however, by ultrasonography because ultrasonography is slightly better at finding gallstones and can be done immediately without waiting one or two days for the iodine to be absorbed, excreted, and concentrated.
Unlike ultrasonography, the OCG also cannot give information about the presence of non-gallstone-related diseases. As would be expected, ultrasonography sometimes finds gallstones that are missed by the OCG. Less frequently, the OCG finds gallstones that are missed by ultrasonography. For this reason, if there is a strong suspicion that gallstones are present, but ultrasonography does not show them, it is reasonable to consider doing an OCG; however, EUS has mostly replaced the OCG in this situation.
An OCG should not be done in individuals who are allergic to iodine.
Intravenous cholangiogram (IVC)
The intravenous cholangiogram or IVC is a radiologic (X-ray) procedure that is used primarily for looking at the larger intrahepatic and extrahepatic bile ducts. It can be used to locate gallstones within these ducts.
An iodine-containing dye is injected intravenously into the blood. The dye is removed from the blood by the liver and excreted into the bile. Unlike the iodine used in the OCG, the iodine in the IVC is concentrated sufficiently enough in the bile ducts to outline the ducts and any gallstones within them. The IVC is rarely used because it has been replaced by MRI cholangiography and endoscopic ultrasound. Moreover, occasional serious reactions to the iodine-containing dye can occur, which rarely may result in the death of the patient.
Complications of gallbladder stones or cholelithiasis include cholangitis, gangrene of the gallbladder, jaundice, pancreatitis, sepsis, fistula, and ileus.
Gallbladder sludge is associated with symptoms and complications of gallstones; however, like gallstones, sludge usually does not cause problems.
The best single test for diagnosing gallstones is transabdominal ultrasonography. Other tests include endoscopic ultrasonography, magnetic resonance cholangiopancreatography (MRCP), Chole scintigraphy (HIDA scan), endoscopic retrograde cholangiopancreatography (ERCP), liver and pancreatic blood tests, duodenal drainage, oral Chole cystogram (OCG), and intravenous cholangiogram (IVC).
Gallbladder stones or cholelithiasis are blamed for many symptoms they do not cause. Among the symptoms gallstones do not cause are:
- dyspepsia (including abdominal bloating and discomfort after eating),
- intolerance to fatty foods,
- belching, and
- flatulence (passing gas or farting).
Allopathic Treatment for Gallbladder stones or cholelithiasis
Gallbladder stones or cholelithiasis are managed primarily with observation (no treatment) or removal of the gallbladder (cholecystectomy). Less commonly used treatments include sphincterotomy and extraction of gallstones, dissolution with oral medications, and extracorporeal shock-wave lithotripsy (ESWL). Prevention of cholesterol gallstones also is possible with oral medications.
- If silent gallstones are discovered in an individual at age 65 (or older), the chance of developing symptoms from the gallstones is only 20% (or less) assuming a life span of 75 years. In this instance, it is reasonable not to treat the individual.
- In younger individuals, no treatment also may be appropriate if the individuals have serious, life-threatening diseases, for example, serious heart disease, that is likely to shorten their life span.
- On the other hand, in healthy young individuals, treatment should be considered even for silent gallstones because the individual chances of developing symptoms from the gallstones over a lifetime will be higher. Once symptoms begin, treatment should be recommended since further symptoms are likely, and more serious complications can be prevented.
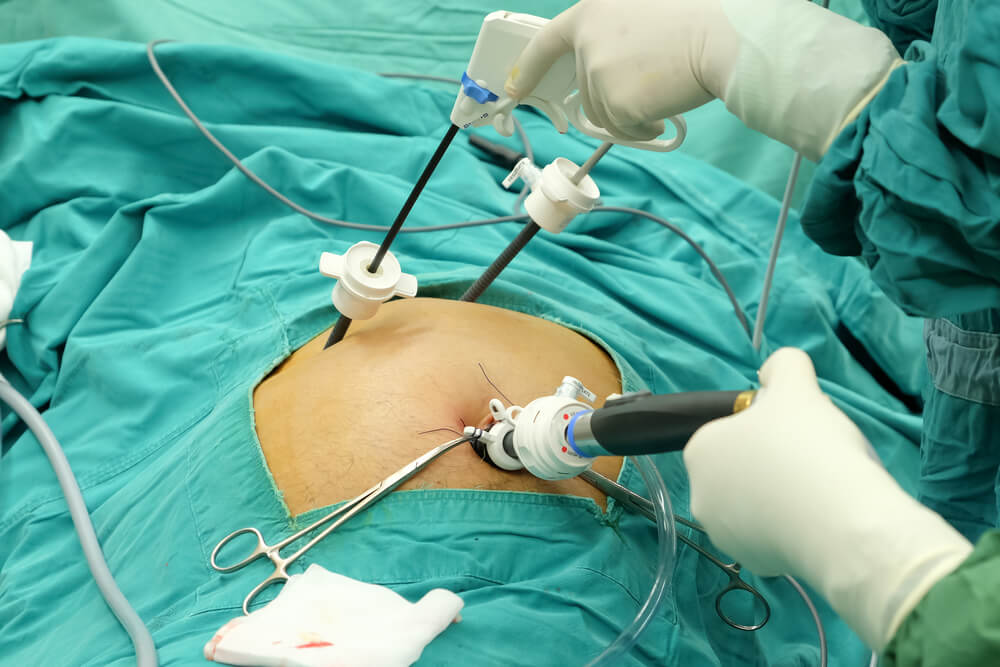
Cholecystectomy
Cholecystectomy (removal of the gallbladder surgically) is the standard treatment for gallstones in the gallbladder. Surgery may be done through a large abdominal incision, laparoscopically, or robotically through small punctures in the abdominal wall. Laparoscopic surgery results in less pain and a faster recovery. Robot-assisted laparoscopic surgery has 3D visualization. Cholecystectomy has a low rate of complications, but serious complications such as damage to the bile ducts and leakage of bile occasionally occur. There also is risk associated with the general anesthesia that is necessary for either type of surgery. Problems following removal of the gallbladder are few. Digestion of food is not affected, and no change in diet is necessary. Nevertheless, chronic diarrhea occurs in approximately 10% of patients.
Sphincterotomy and extraction of Gallbladder stones or cholelithiasis
Sometimes a gallbladder stone or cholelithiasis may be stuck in the hepatic or common bile ducts. In such situations, there usually are gallstones in the gallbladder as well, and cholecystectomy is necessary. It may be possible to remove the gallstone stuck in the duct at the time of surgery, but this may not always be possible. An alternative means for removing gallstones in the duct before or after cholecystectomy is with sphincterotomy followed by extraction of the gallstone.
Sphincterotomy involves cutting the muscle of the common bile duct (sphincter of Oddi) at the junction of the common bile duct and the duodenum in order to allow easier access to the common bile duct. The cutting is done with an electrosurgical instrument passed through the same type of endoscope that is used for ERCP. After the sphincter is cut, instruments may be passed through the endoscope and into the hepatic and common bile ducts to grab and pull out the gallstone or to crush the gallstone.
It also is possible to pass a lithotripsy instrument that uses high-frequency sound waves to break up the gallstone. Complications of sphincterotomy and extraction of gallstones include risks associated with general anesthesia, perforation of the bile ducts or duodenum, bleeding, and pancreatitis.
Oral dissolution therapy
It is possible to dissolve some cholesterol gallstones with medication taken orally. The medication is a naturally occurring bile acid called ursodeoxycholic acid or ursodiol. Bile acids are one of the detergents that the liver secretes into bile to dissolve cholesterol. Although one might expect therapy with ursodiol to work by increasing the number of bile acids in bile and thereby cause the cholesterol in gallstones to dissolve, the mechanism of ursodiol’s action actually is different. Ursodiol reduces the amount of cholesterol secreted in bile. The bile then has less cholesterol and becomes capable of dissolving the cholesterol in the gallstones.
There are important limitations to the use of ursodiol:
- It is only effective for cholesterol gallstones and not pigment gallstones.
- It works only for small gallstones, less than 1-1.5 cm in diameter.
- It takes one to two years for the gallstones to dissolve, and many of the gallstone’s reform following cessation of treatment.
Due to these limitations, ursodiol generally is used only in individuals with smaller gallstones that are likely to have a very high cholesterol content and who are at high risk for surgery because of ill health. It also is reasonable to use ursodiol in individuals whose gallstones were perhaps formed because of a transient event, for example, the rapid loss of weight, since the gallstones would not be expected to recur following successful dissolution. Another use of ursodiol is to prevent the formation of gallstones in patients who will lose weight rapidly.
Extracorporeal shock-wave lithotripsy
Extracorporeal shock-wave lithotripsy (ESWL) is an infrequently used method for treating gallstones, particularly those lodged in bile ducts. ESWL generators produce shock waves outside of the body that is then focused on the gallstone. The shock waves shatter the gallstone, and the resulting pieces of the gallstone either drain into the intestine on their own or are extracted endoscopically. Shock waves also can be used to break up gallstones via special catheters passed through an endoscope at the time of ERCP.
Homeopathic Treatment for Gallbladder stones or cholelithiasis
Calcarea Carbonica
Sensitive to slightest pressure. Liver region painful when stooping. Cutting in abdomen; swollen abdomen. Incarcerated flatulence. Inguinal and mesenteric glands swollen and painful. Cannot bear tight clothing around the waist. Distention with hardness. Gallbladder stones or cholelithiasis. Glandular swellings. Gall-stone colic. Increase of fat in abdomen. Peritonitis.
Phosphorus
Sensation of heat in the back between shoulder-blades. Sharp pains in hepatic region. Acute yellow atrophy of the liver. Enlargement and induration of liver. Enlargement of spleen. Inflammation of intestines. Acute hepatitis. Fatty degeneration. Jaundice.
Lycopodium Clavatum
Biliousness. Constipation. Cystitis. Fibroma. Flatulence. Gallbladder stones or cholelithiasis and colic, Violent gall-stone colic. Glands swelling. Heart diseases. Liver diseases. Mouth clammy or bitter. Inability to digest heavy food. After a meal, hepatic pains. Sourness and diarrhea after taking milk.
Cholesternium
Gallstones and gallstone colic. Gallbladder stones or cholelithiasis and insomnia. Liver diseases.
Colocynthis
Gallbladder stones or cholelithiasis colic. Agonizing cutting, shooting pain. Constant nausea with risings, greenish and/or bitter vomiting. Bitter taste in the mouth, and of all food and drink. Colic and diarrhea. Severe pain in liver region. Gallbladder infection.
Dioscorea Villosa
Severe pain. Hard, dull pain, gallbladder. Cutting, squeezing pain, twisting pain. Colic begins at umbilicus and radiates to all parts of body. Eructation of sour, bitter wind, with hiccough. Sharp pain in epigastrium. Pain from gallbladder to chest, back, and arms.
Chelidonium Majus
Colic, navel drawn in.-Stitches in liver and spleen. Shooting stitching through liver to back; crampy pain inner angle of scapula, pain through stomach to back and right shoulder-blade. Gastralgia. Hypochondrium and scrobiculus cordis tense and painful on pressure. Pains across umbilicus as if abdomen constricted by a string. Abdominal plethora; distension, rumbling. Tongue yellow, with imprint of teeth; large and flabby. Taste bitter, pasty. Bad odor from mouth. Jaundice due to hepatic and gallbladder obstruction. Gallbladder stones or cholelithiasis. Gall-colic. Distention. Fermentation and sluggish bowels. Constriction across, as by a string. Liver enlarged.
Fel Tauri
Gallstones. Obstruction of the gall ducts. Fel tauri increases the duodenal secretion, emulsifies fat and increases the action of the intestines. Liquefies bile and removes the obstruction of gall ducts.
Ceanothus Americanus
Loss of appetite. Thirst for water, but it made him sick. Deep-seated abdominal pain can’t sit or to lai. Enormous enlargement of the spleen. Splenitis; pain all up the left side. Deep-seated pain in left hypochondrium, hypertrophy of spleen. Leukemia. Gallbladder stones or cholelithiasis. Gallbladder diseases. Gallbladder swelling. Polyuria, urine with greenish mucus, with bile. Diabetes.
Nux vomica
Bilious attack. Breath sour. Constipation. Dyspepsia. Gallbladder stones or cholelithiasis. Gastrodynia. Liver diseases. Food/meals, milk feels acidic taste. Vomiting sore. Sore or bitter eructation.
China sulphuricum
Mouth taste bitter, sometimes with a clean tongue; clammy, sickly; earthy; empyreumatic. Bread appears bitter. Bitter hiccough and retching. Nausea with risings (empty or bitter). In the hepatic region, pains sometimes increasing towards evening, feels better with pressure. Swelling and hardness of the splenic and hepatic regions, with lancinations, especially on breathing deeply, sneezing, coughing etc.
China Officianalis
Vomiting of undigested food. Obstruction in gallbladder with colic, periodic recurrence. Biliary calculi. Intensely sensitive to touch, to motion, to cold air. Periodicity, pains come on regularly at a given time each day, or every night at 12 o’ clock. Drenching night sweats. Pain more at night. Vomiting of undigested food. Belching of bitter fluid or regurgitation of food gives no relief. Pain in the hepatic region, worse from touch. Shooting in region of liver, tenderness and pain on touching the part. Liver region sensitive to least pressure. Abdomen is bloated with excess of gas, painful distension of abdomen. Tympanitic abdomen. Pain in right hypochondrium. Gallbladder stones or cholelithiasis. Gallstone colic.
Hydrangea Arborescens
Hydrangea has a traditional reputation as a “stone-breaking” medicine having been used in calculous diseases for many years in Arab and Asian countries. It also acts like diuretic, painkiller (anesthetic) and vasodilator. Gallbladder stones or cholelithiasis.
Berberis Vulgaris
Biliary colic. Bilious attack/Jaundice. Calculus. Gallbladder stones or cholelithiasis. Gravel/renal stones. Liver and/or spleen diseases. Mouth taste bitter. Morning vomiting. Constipation like sheep dung.
Thuja Occidentalis
Granular inflammation. Fatty tumors. Complete loss of appetite. cutting pain in abdomen.
Chionanthus Virgenica
Gallstone colic. Gallbladder stones or cholelithiasis. Better lying on abdomen. Colic with cold sweat on forehead. Hypertrophy of liver. Jaundice. Loss of appetite. Nausea and retching with desire for stool. Tongue heavily coated. Bitter, sour, hot, bilious, ropy, gushing, vomiting, sets the teeth on edge. It is a remedy for the expulsion of stones, also a preventive for the formation of stones.
Pulsatilla
Vomitings, sometimes violent, of greenish mucus, or bilious and bitter, or acid matter. Gallbladder diseases. Gallbladder stones or cholelithiasis.
Atista Indica
Colic pain around the umbilicus which makes the patient senseless. Pain worse after eating and is relieved by-passing flatus. Nausea aggravates in morning. Canine hunger and desire for sweets. Bitter taste in mouth. Helps in relieving colic pain, Effective in biliary and gastric problems, Useful in treating dysentery and diarrhea, helps in curing cold and tonsillitis, helps in curing bleeding gums and pain in the teeth, soothes nausea and vomiting, helps in loose motions and reduces numbness.
Cactus Grandiflorus
Gallbladder stones or cholelithiasis with constriction and cardiac affections. Colic after meals. Morning nausea and vomiting.
Hydrastis Canadensis
Gallbladder stones or cholelithiasis. Catarrhal inflammation of mucous lining of gallbladder and biliary ducts. Cutting pain from liver to right scapula, worse lying on back or right side. Fullness and tenderness over liver region. Stools, white and frequent. Bitter, peppery taste in mouth. Jaundice, yellow skin. Constipation.
Leptandra Virginica
Gallbladder stones or cholelithiasis. Gallbladder pain. Burning in liver region. Sore, dull, burning ache over liver or near gallbladder. Jaundice. Bilious attack. Bilious fever. Yellow coated tongue. Craving for cold drinks which aggravates burning and aching in stomach. profuse, black, fetid stools
Thlaspi Bursa Pastoris
Gallbladder stones or cholelithiasis. Gallstone colic. Liver affections secondary to uterine conditions.
Veratrum Album
Gallstone colic. Gallbladder stones or cholelithiasis. Great pressure on liver region with vomiting and diarrhea. Profuse sweating, cold sweat on forehead. Hyperemia of liver. Cold skin, cold face, cold back, cold hands, feet and legs, cold sweat.
Merc Sole
Gallstone colic. Gallbladder stones or cholelithiasis. Violent stitches in hepatic region, could not breathe or eructate. Worse night. Cannot lie on right side. Jaundice. Bad taste in mouth. Tongue moist and furred. Profuse salivation. Fetid odor from mouth. Profuse sweat, but does not relieve, may even increase the suffering.
Morgan Gaertner
Gallstone colic. Relieve pain, also dissolve the stone. Gallbladder stones or cholelithiasis. 
Podophyllum Peltatum
Jaundice with gallstones. Sore and painful liver, better rubbing. Liver and whole abdominal viscera are sore. Colic at daylight every morning. Better bending forward, warmth application. Tongue yellow or white, shows the imprint of teeth. Gallbladder stones or cholelithiasis.
Stigmata Madagus
Gallstone colic. Gallbladder stones or cholelithiasis. Relieves at once the violent pain if given during paroxysm.
Terminalia Chebula
Intense pain in abdomen, aggravated at night. Pain aggravated by sitting, better by lying down. Flatulence and distension of abdomen, relieved by-passing flatus. Anorexia, profuse salivation, and bitter taste in mouth. Tongue is coated brown. Gallbladder stones or cholelithiasis.
P. S: This article is only for doctors having good knowledge about Homeopathy and allopathy, for learning purpose(s).
For proper consultation and treatment, please visit our clinic.
None of above-mentioned medicine(s) is/are the full/complete treatment but just hints for treatment; every patient has his/her own constitutional medicine.
 Dr. Sayyad Qaisar Ahmed (MD {Ukraine}, DHMS), Abdominal Surgeries, Oncological surgeries, Gastroenterologist, Specialist Homeopathic Medicines.
Dr. Sayyad Qaisar Ahmed (MD {Ukraine}, DHMS), Abdominal Surgeries, Oncological surgeries, Gastroenterologist, Specialist Homeopathic Medicines.
Senior research officer at Dnepropetrovsk state medical academy Ukraine.
Location: Al-Haytham clinic, Umer Farooq Chowk Risalpur Sadder (0923631023, 03119884588), K.P.K, Pakistan.
Find more about Dr Sayed Qaisar Ahmed at:
https://www.youtube.com/Dr Qaisar Ahmed



That is a really good tip especially to those new to the blogosphere. Brief but very precise info… Many thanks for sharing this one. A must read article!
🥰
Thank you, I have recently been looking for information approximately this subject for a while and yours is the greatest I have came upon so far. But, what in regards to the conclusion? Are you sure about the supply?
Thank you for all your valuable work on this web site. Betty really loves managing internet research and it’s really easy to understand why. A lot of people hear all regarding the dynamic way you present priceless guidance through your web blog and in addition foster contribution from other people on that content and our favorite simple princess is really becoming educated a lot. Take advantage of the rest of the year. You are conducting a remarkable job.
Wow, marvelous blog layout! How long have you been blogging for? you make blogging look easy. The whole glance of your site is excellent, let alone the content material!
Hello, i think that i saw you visited my blog thus i came to 搑eturn the favor?I’m attempting to find things to enhance my site!I suppose its ok to use some of your ideas!!
I feel this is among the so much important information for me. And i’m happy reading your article. But wanna observation on few normal issues, The website style is ideal, the articles is in point of fact great : D. Excellent activity, cheers
Excellent read, I just passed this onto a friend who was doing a little research on that. And he just bought me lunch since I found it for him smile So let me rephrase that: Thank you for lunch!
Wow, incredible weblog layout! How long have you been running a blog for? you make running a blog look easy. The total look of your website is excellent, let alone the content!
The articles you write help me a lot and I like the topic
I am glad to be a visitor of this sodding site! , appreciate it for this rare info ! .
Only wanna admit that this is very helpful, Thanks for taking your time to write this.
wonderful points altogether, you simply received a brand new reader. What may you recommend about your post that you just made a few days in the past? Any positive?
My partner and I absolutely love your blog and find the majority of your post’s to be exactly what I’m looking for. Do you offer guest writers to write content for you personally? I wouldn’t mind producing a post or elaborating on a lot of the subjects you write related to here. Again, awesome weblog!