Osteomyelitis is inflammation of the bone caused by an infecting organism. Although bone is normally resistant to bacterial colonization, it can become infected in multiple ways. The infecting organism may reach bone through blood or as a consequence of events such as trauma, surgery, the presence of foreign bodies, or the placement of prostheses that disrupt bony integrity and predispose to the onset of bone infection.
When prosthetic joints are associated with infection, microorganisms typically grow in biofilm, which protects bacteria from allopathic antimicrobial treatment and the host immune response, but Homeopathic medicines can reach that places and even into the axial skeleton, auditory ossicles and the appendicular skeleton. Osteomyelitis can be acute, subacute, or chronic, depending on its duration.
Anatomy
The bony skeleton is divided into two parts: the axial skeleton and the appendicular skeleton. The axial skeleton is the central core unit, consisting of the skull, vertebrae, ribs, and sternum; the appendicular skeleton comprises the bones of the extremities. The human skeleton consists of 213 bones, of which 126 are part of the appendicular skeleton, 74 are part of the axial skeleton, and six are part of the auditory ossicles.
Hematogenous osteomyelitis most commonly involves the vertebrae, but infection may also occur in the metaphysis of the long bones, pelvis, and clavicle. Vertebral osteomyelitis usually involves two adjacent vertebrae with the corresponding intervertebral disk. The lumbar spine is most commonly affected, followed by the thoracic and cervical regions. A form of hematogenous osteomyelitis that is more common occurs in infants and children and develops in the metaphysis.
Posttraumatic osteomyelitis begins outside the bony cortex and works its way in toward the medullary canal; it is typically found in the tibia but can occur in any bone. Contiguous-focus osteomyelitis often occurs in the bones of the feet in patients with diabetes mellitus and vascular compromise.
Pathophysiology
Bone is normally resistant to infection. However, when microorganisms are introduced into bone hematogenously from surrounding structures or from direct inoculation related to surgery or trauma, osteomyelitis can occur. Bone infection may result from the treatment of trauma, which allows pathogens to enter bone and proliferate in the traumatized tissue. When bone infection persists for months, the resulting infection is referred to as chronic osteomyelitis and may be polymicrobial. Although all bones are subject to infection, the lower extremity is most commonly involved.
Important factors in the pathogenesis of osteomyelitis include the following:
-
Virulence of the infecting organism,
-
Underlying disease,
-
Immune status of the host,
Bacteria may possess various factors that may contribute to the development of osteomyelitis. For example, factors promoted by S aureus may promote bacterial adherence, resistance to host defense mechanisms, and proteolytic activity.
Hematogenous osteomyelitis
In adults, the vertebrae are the most common site of hematogenous osteomyelitis, but infection may also occur in the long bones, pelvis, and clavicle.
Primary hematogenous osteomyelitis is more common in infants and children, usually occurring in the long-bone metaphysis. However, it may spread to the medullary canal or into the joint. When infection extends into soft tissue, sinus tracts eventually will form. Secondary hematogenous osteomyelitis is more common and can develop from any primary focus of infection or from reactivation of a previous infection in the presence of immunocompromised status. In adults, the location is also usually metaphyseal.
In the long bones, the blood supply penetrates the bone at the midshaft but then splits into two segments traveling to each metaphyseal endplate. These vessels are terminal, and bacteria enter through the nutrient artery and lodge at the valveless capillary loops in the junction between the metaphysis and the physis. The blood flow through capillary loops and sinusoidal veins at the epiphyseal-metaphyseal junction is very slow, allowing the bacteria to establish and proliferate. This region does not permit good penetration of white blood cells and other immune mediators, thus serving to protect the bacteria.
Bacteria
As the bacteria continue to multiply, the scarce functioning phagocytes release enzymes that lyse the bone, thereby creating an inflammatory response. This results in formation of pus (a protein-rich exudate containing dead phagocytes, tissue debris, and microorganisms), increasing the intramedullary pressure in the area and thus further limiting the already compromised blood supply. The stasis and cytokine activity promote clot formation in the blood vessels, leading to bone ischemia and then necrosis.
Infection then spreads into the vortex through the Haversian system and Volkmann canals and finally into the subperiosteal space. The infection and the formation of pus in this region strip the periosteum from the shaft and stimulate an osteoblastic response. As a result, new bone is formed in response to the periosteal stripping. Part of the necrotic bone may separate; this is referred to as the sequestra. In a severe infection, the entire shaft is encased in a sheath of new bone, which is referred to as the involucrum. Once this occurs, a major part of the shaft has been deprived of its blood supply.The involucrum can have openings called cloacae, which allow pus to escape from the bone, leading to fulminant disease.
S aureus is the pathogenic organism most commonly recovered from bone, followed by Pseudomonas and Enterobacteriaceae. Organisms less commonly involved include anaerobe gram-negative bacilli. Intravenous (IV) drug users may acquire pseudomonal infections. Gastrointestinal or genitourinary infections may lead to osteomyelitis involving gram-negative organisms. Dental extraction has been associated with viridans streptococcal infections.
Contiguous-focus and posttraumatic osteomyelitis
The initiating factor in contiguous-focus osteomyelitis often consists of direct inoculation of bacteria via trauma, surgical reduction and internal fixation of fractures, prosthetic devices, spread from soft-tissue infection, spread from adjacent septic arthritis, or nosocomial contamination. Infection usually results approximately 1 month after inoculation.
Posttraumatic osteomyelitis more commonly affects adults and typically occurs in the tibia. The most commonly isolated organism is S aureus. At the same time, local soft-tissue vascularity may be compromised, leading to interference with healing. Compared with hematogenous infection, posttraumatic infection begins outside the bony cortex and works its way in toward the medullary canal. Low-grade fever, drainage, and pain may be present. Loss of bone stability, necrosis, and soft-tissue damage may lead to a greater risk of recurrence. 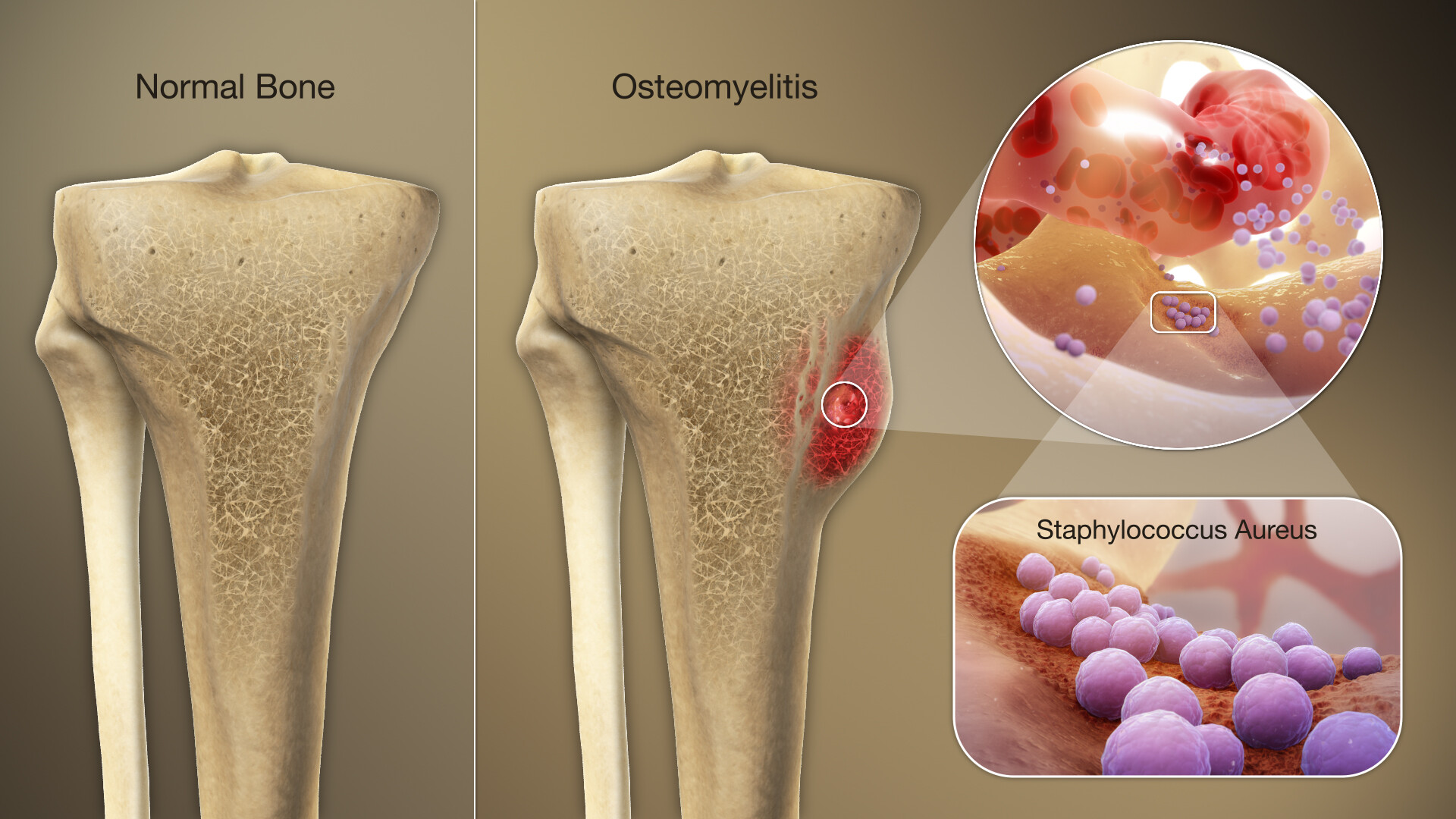
Septic arthritis
Septic arthritis may lead to osteomyelitis. Abnormalities at the joint margins or centrally, which may arise from overgrowth and hypertrophy of the synovial pannus and granulation tissue, may eventually extend into the underlying bone, leading to erosions and osteomyelitis. One study demonstrated that septic arthritis in elderly persons most commonly involves the knee and that, despite most of the patients having a history of surgery, 38% developed osteomyelitis.
Septic arthritis is more common in neonates than in older children and is often associated with metaphyseal osteomyelitis. Although rare, gonococcal osteomyelitis may arise in a bone adjacent to a chronically infected joint. In children the intra-articular position of some metaphysis makes them prone to the development of secondary septic arthritis (eg, in the knee, hip, or shoulder).
Many patients with vascular compromise, as in diabetes mellitus, are predisposed to osteomyelitis owing to an inadequate local tissue response.
Infection in neuropathic or vascular-compromised feet is most often caused by minor trauma to the feet with multiple organisms isolated from bone, including Streptococcus species, Enterococcus species, coagulase-positive and -negative staphylococci, gram-negative bacilli, and anaerobic organisms. Fungal infections are also known in neuropathic feet with osteomyelitis. Foot ulcers allow bacteria to reach the bone. Patients may not experience any resulting pain, because of peripheral neuropathy, and may present with a perforating foot ulcer, cellulitis, or an ingrown toenail.
Vertebral osteomyelitis
The incidence of vertebral osteomyelitis generally increases progressively with age, with most affected patients being older than 50 years. Although devastating complications may result from a delay in diagnosis, vertebral osteomyelitis has rarely been fatal since the development of antibiotics. However, the elderly have higher rates of bacteremia and infective endocarditis at the time of diagnosis, and they have a higher mortality than younger patients with osteomyelitis do.
The infection usually originates hematogenously and generally involves two adjacent vertebrae with the corresponding intervertebral disk. The lumbar spine is most commonly affected, followed by the thoracic and cervical regions.
Potential sources of infection include skin, soft tissue, respiratory tract, genitourinary tract, infected intravenous (IV) sites, and dental infections. S aureus is the most commonly isolated organism. However, Pseudomonas aeruginosa is more common in IV drug users.
Most patients with vertebral osteomyelitis present with localized pain and tenderness of the involved vertebrae with a slow progression over 3 weeks to 3 months. Fever may be present in approximately 50% of patients. Some 15% of patients may have motor and sensory deficits. Laboratory studies may reveal peripheral leukocytosis and an elevated erythrocyte sedimentation rate (ESR). Extension of the infection may lead to abscess formation.
Osteomyelitis in children
Acute hematogenous osteomyelitis usually occurs after an episode of bacteremia in which the organisms inoculate the bone. The organisms most commonly isolated in these cases include S aureus, Streptococcus pneumoniae, and Haemophilus influenza type b (less common since the use of vaccine for H influenza type b). The incidence of Kinsella kingae infection is increasing; such infection is a common cause of osteomyelitis in children younger than 4 years.
Acute hematogenous S aureus osteomyelitis in children can lead to pathologic fractures. This can occur in about 5% of cases, with a 72-day mean time from disease onset to fracture.
In children with subacute focal osteomyelitis (see the image below), S aureus is the most commonly isolated organism.
 Rarefaction and periosteal new-bone formation around the left upper fibula in a 12-year-old patient. This was caused by subacute osteomyelitis.
Rarefaction and periosteal new-bone formation around the left upper fibula in a 12-year-old patient. This was caused by subacute osteomyelitis.
Gram-negative bacteria such as Pseudomonas species or Escherichia coli are common causes of infection after puncture wounds of the feet or open injuries to bone. Anaerobes can also cause bone infection after human or animal bites.
Osteomyelitis in the neonate results from hematogenous spread, especially in patients with indwelling central venous catheters. The common organisms in osteomyelitis of the neonate include those that frequently cause neonatal sepsis—namely, group B Streptococcus species—and E coli. Infections in the neonate can involve multiple osseous sites, and approximately half of the cases also involve eventual development of septic arthritis in the adjacent joint.
Children with sickle cell disease are at an increased risk for bacterial infections, and osteomyelitis is the second most common infection in these patients. The most common organisms involved in osteomyelitis in children with sickle cell anemia include Salmonella species, S aureus, Serratia species, and Proteus mirabilis.
Physical Examination
On physical examination, scars or local disturbance of wound healing may be noted along with the cardinal signs of inflammation. Range of motion (ROM), deformity, and local signs of impaired vascularity are also sought in the involved extremity. If periosteal tissues are involved, point tenderness may be present.
Complications
The most common complication in children with osteomyelitis is recurrence of bone infection. Complications as a result of acute hematogenous osteomyelitis due to methicillin-resistant S aureus (MRSA) is often attributed to more complicated illness, as compared with osteomyelitis caused by methicillin-sensitive S aureus (MSSA) or any other organism. Potential complications of osteomyelitis include the following:
-
Septic pulmonary emboli,
-
Deep vein thrombosis in the region near the infected bone,
-
Intraosseous and subperiosteal abscess,
-
Pathologic fracture – This is a rare complication and can occur as a result of extreme bone destruction or thinning of the cortex,
-
Growth disturbance when epiphyseal plate is involved,
Adverse outcomes are common with delayed treatment; however, even when appropriate treatment is provided, chronic infection may still develop in 5-10% of cases. Chronic osteomyelitis presents 6 weeks or longer after a bone infection, and its characteristics include bone destruction and formation of sequestra. Leading complications resulting from chronic osteomyelitis include sinus tracts and extension to adjacent structures, as well as abscess formation. One complication that must not be missed is malignant transformation (ie, Marjolin ulcer). This typically has a latency period of 27-30 years from the initial onset of osteomyelitis, and it involves aggressive squamous cell carcinoma (SCC).
Diagnostic Considerations
Crystal arthropathies (gout and pseudogout) presents in a similar manner to septic arthritis. The diagnosis can be made by means of polarized microscopic examination of monosodium urate crystals in gout or calcium pyrophosphate crystals in pseudogout.
In children, Ewing sarcoma is a common form of bone malignancy. It presents with clinical symptoms of fever, pain, malaise, and swelling, which are very similar to those of osteomyelitis. Invasion of the tumor into the periarticular space is uncommon but, if present, can radiographically mimic septic arthritis.
Septic arthritis generally presents with acute pain, swelling, warmth, and decreased range of motion (ROM) in a single joint. Only 40-60% of patients will have a fever at presentation. Laboratory studies and synovial fluid analysis are helpful for diagnosis. The demarcation between the two can be often difficult and requires careful clinical examination and, sometimes, arthrocentesis to test joint fluid.
In patients with sickle cell disease, it can be challenging to differentiate between a vaso-occlusive crisis and an infection such as osteomyelitis. An infectious etiology is less likely if more than one area of the body is affected. Osteomyelitis also tends to have clinical symptoms (eg, pain, swelling, and fever) developing over a longer time course than a vaso-occlusive crisis.
Clinical suspicion, presence of deep bony tenderness, local signs of inflammation, and symptoms of acute clinical infection are helpful in initiating a diagnosis of acute osteomyelitis where radiologic signs may be absent or minimal and time is of the essence.
Diagnosis and Tests
How do providers diagnose osteomyelitis?
A healthcare provider will diagnose osteomyelitis with a physical exam and some tests. They’ll ask about your symptoms and when you first noticed them. Tell your provider if you’ve recently had surgery, an injury or if you’ve started new treatments for other health conditions.
Your provider will use some of the following tests to diagnose the infection and take pictures of your bones:
- Blood tests.
- X-ray.
- Magnetic resonance imaging (MRI).
- Computed tomography (CT) scan.
- Ultrasound.
- Bone scan.
- Bone marrow biopsy. 
Allopathic therapy
Allopathic antibiotic treatment should be based on the identification of pathogens from bone cultures at the time of bone biopsy or debridement. Bone cultures are obtained first, and suspected pathogens are then covered by initiation of a parenteral antimicrobial treatment. However, allopathic treatment may be modified once the organism is identified. Parenteral and oral antibiotics may be used alone or in combination, depending on microorganism sensitivity results, patient compliance, and infectious disease consultation.
Prophylactic treatment with the bead pouch technique has been suggested in open fractures to reduce the risk of infection. Systemic antibiotics supplemented with antibiotic beads are preferred to systemic antibiotics alone.
Prolonged antibiotic therapy is the cornerstone of treatment for osteomyelitis. Results of culture and sensitivity should guide antibiotic treatment, if possible, but in the absence of this data, it is reasonable to start empiric antibiotics. A commonly used broad-spectrum empiric antibiotic regimen against both gram-positive and negative organisms, including MRSA, is vancomycin (15 mg/kg intravenously [IV] every 12 hours) plus a third a generation cephalosporin (e.g., ceftriaxone 2 gm IV daily) or a beta-lactam/beta-lactamase inhibitor combination (e.g., piperacillin/tazobactam 3.375 IV every 8 hours). Once sensitivity data becomes available, then the antibiotic therapy should be narrowed for targeted coverage of the susceptible organisms.
Local antibiotics
Local antibiotic therapy with gentamicin-impregnated Septopal beads. Factors involved in the debate include the length of implantation, the need for removal, and the choice of nonabsorbable versus bioabsorbable delivery vehicles. Prolonged implantation of antibiotic beads and spacers remains controversial owing to the risk of secondary infection and development of resistant organisms. Secondary infection stems from the beads, which may serve as a foreign body upon complete elution of antibiotic.
Traditionally, allopathic antibiotic treatment of osteomyelitis has consisted of a 4- to 6-week course. Animal studies and observations show that bone revascularization following debridement takes about 4 weeks. However, if all infected bone is removed, as in forefoot osteomyelitis, antibiotic therapy can be shortened to 10 days.
Oral antibiotics
Oral antibiotics that have been proved to be effective include clindamycin, rifampin, trimethoprim-sulfamethoxazole, and fluoroquinolones. Clindamycin is given orally after initial intravenous (IV) treatment for 1-2 weeks and has excellent bioavailability. It is active against most gram-positive bacteria, including staphylococci. Linezolid is active against methicillin-resistant staphylococci and vancomycin-resistant Enterococcus. It inhibits bacterial protein synthesis, has excellent bone penetration, and is administered IV or orally.
Oral quinolones are often used in adults for gram-negative organisms. Rifampin has an optimal intercellular concentration and a good sensitivity profile for methicillin-resistant staphylococci. It is used in combination with cell wall–active antibiotics to achieve synergistic killing and to avoid rapid emergence of resistant strains. 
Empiric therapy
Empiric therapy is necessary when it is not possible to isolate organisms from the infection site. Hospital-acquired infections are usually derived from methicillin-resistant staphylococci. Infections contracted outside the hospital are often polymicrobial with the presence of gram-negative bacteria.
Infection may fail to improve, owing to the ability of bacteria to resist antibiotics. Some bacteria, such as S epidermidis in prosthesis infections, adhere to a biofilm that protects the organism from phagocytosis and impedes delivery of the antibiotic. The use of rifampin in combination with other antibiotics has been found to be more effective than monotherapy for treating infection associated with surgical hardware.
Suppressive antibiotic therapy should also be directed by bone culture and is given orally when surgery is contraindicated. If the infection recurs after 6 months of suppressive antibiotic treatment, a new lifelong regimen of suppressive therapy may be tried.
With allopathic treatment surgical debridement of all diseased bone is often required as antibiotics penetrate poorly into infected fluid collections such as abscesses and injured or necrotic bone.
Also important is the need for revascularization of the affected limb before surgical intervention if there is evidence of significant peripheral vascular disease, control diabetes mellitus and address other host factors that may impede wound healing, including tobacco use, malnutrition, chronic hypoxia, immunodeficiency states, chronic lymphedema and peripheral neuropathy.
Homeopathic Treatment for osteomyelitis
Good bioavailability, lowest toxicity, and adequate bone penetration are important factors in treatment. With Homeopathic treatment there is no need for surgical debridement of diseased bone is required as Homeopathic antibiotics and anti-fungal medicines penetrate very well into infected fluid collections such as abscesses and injured or necrotic bone. Homeopathic antibiotic treatment should be based on the identification of pathogens from bone cultures at the time of bone biopsy or debridement.
Oral Homeopathic medicines may be used alone or in combination (better), prophylactic treatment has been suggested in open fractures to reduce the risk of infection.
Here are some Homeopathic antibiotics and anti-fungal medicines:
Arnica Montana
Injuries, falls, blows, contusions. Tinnitus aurum. Putrid phenomena. Septic conditions; prophylactic of pus infection. Apoplexy. Strains. Arnica is disposed to cerebral congestion. Acts best in plethoric, feebly in debilitated with impoverished blood, cardiac dropsy with dyspnea. Tendency to hemorrhage and low-fever states. Tendency to tissue degeneration, septic conditions, abscesses that do not mature. Neuralgia. Infections in muscles and tendons. Abcesses.
Bellis Perennis
Septic conditions. Severe muscular soreness. It acts upon the muscular fibers of the blood-vessels. Much muscular soreness. Lameness, as if sprained. Venous congestion, due to mechanical causes. First remedy in injuries to the deeper tissues, after major surgical work. Results of injuries to nerves with intense soreness and intolerance of cold bathing. Traumatism of the pelvic organs.
Hamamelis Virginia
Venous congestion, hemorrhages, varicose veins, and hemorrhoids, with bruised soreness of affected parts, are the special sphere of this remedy. Acts upon the coats of the veins causing relaxation with consequent engorgement. Passive venous hemorrhages from any part. Great value in open, painful wounds, with weakness from loss of blood. After operations, supersedes the use of morphia. Neuralgia of internal saphenous nerve. 
Rhus Toxicodendron
The effects on the skin, rheumatic pains, mucous membrane affections, affects fibrous tissue markedly-joints, tendons, sheaths-aponeurosis, etc. Post-operative complications. Tearing asunder pains. Septic conditions. Cellulitis and infections. Septicemia.
Myristica Sebifera
A remedy of great antiseptic powers. Inflammation of skin, cellular tissue and periosteum. Traumatic infections. Parotitis. Fistulas. Carbuncles. Specific action in panaritium. Pain in the fingernails with swelling of the phalanges. Phlegmonous inflammations. Hastens suppuration and shortens its duration. Inflammation of middle ear, suppurative stage. Fistula in ano. Acts more powerfully often than Heper or Silica.
Heper Sulphur
Suits especially scrofulous and lymphatic constitutions who are inclined to have eruptions and glandular swellings. Unhealthy skin. Blondes with sluggish character and weak muscles. Sensitiveness to all impressions. Croupous catarrhal inflammation, profuse secretion; easy perspiration. After abuse of allopathic drugs. Infections with pus forming. The lesions spread by the formation of small papules around the side of the old lesion. Chilliness, hypersensitiveness, splinter-like pains. The side of the body on which he lies at night becomes gradually insufferably painful; he must turn. Pellagra (material doses required). Syphilis after antibiotic gross medication (allopathic).
Mercurius solubilis
Every organ and tissue of the body is affected by this powerful medicine, a useful life saving and life preserving service if employed homeopathically, guided by its clear-cut symptoms. Inflamed and necrotic wrecks, decomposing the blood, profound anemia. The lymphatic system is especially affected with all the membranes and glands, and internal organs, bones etc. Secondary stage of syphilis. Sever pains behind sternum, around joints, etc. Hereditary syphilis manifestations are within its range, bullae, abscesses, snuffles, marasmus, stomatitis or destructive inflammations.
Tremors everywhere. Sensitive to heat and cold. Swellings, with raw, sore feeling; the profuse, oily perspiration does not relieve. Breath, excretions and body smell foul. Tendency to formation of pus, which is thin, greenish, putrid; streaked with thin blood.
Mezereum
Affections of bones, neuralgias, especially about teeth and face. Bruised, weary feeling in joints, with drawing and stiffness. Pains of various kinds, with chilliness and sensitiveness to cold air. Bone pains. Eruptions after vaccination. Burning, darting sensation in the muscles; subsultus tendinous. Pains shoot upward. Semi-lateral complaints. Sensitive to cold air.
Phosphorus
Irritation, inflammation and degeneration of mucous membranes, serous membranes, inflamed spinal cord and nerves (causing paralysis), destroyed bones, especially the lower jaw and tibia. Fatty degeneration of blood vessels and every tissue and organ of the body, hemorrhages, and hematogenous jaundice. 
Destructive metabolism. Nervous debility, emaciation, amative tendencies, sudden prostration, faints, sweats, shooting pains, etc. Polycythemia. Blood extravasations: fatty degenerations, cirrhosis, caries etc. Muscular pseudo-hypertrophy, neuritis. Inflammation of the respiratory tract. Paralytic symptoms. Tertiary syphilis, skin lesions, and nervous debility. Scurvy. Pseudo-hypertrophic paralysis. Ataxia and adynamia. Osteo myelitis. Bone fragility.
Arsenicum Album
A profoundly acting remedy on every organ and tissue. Its clear-cut characteristic symptoms and correspondence to many severe types of disease. Peculiar irritability of fiber. Green discharges. Infantile Kala-azar. Degenerative changes. Septic infections and low vitality.
Bacillinium
Many forms of chronic non-tubercular disease. Consumptiveness Growth, defective. Hydrocephalus. Idiocy. Insanity. Joints, affections of. Phthiriasis. Tubercular inflammation of bone.
Hyppericum Perforatum
The great remedy for injuries to nerves, especially of fingers, toes and nails. Crushed fingers, especially tips. Excessive painfulness. Prevents lockjaw. Punctured wounds. Relieves pain after surgeries. Quite supersedes the use of Morphia after operations. Spasms after every injury. Coccydynia. Injured nerves from bites of animals. Tetanus. Neuritis, tingling, burning and numbness. Constant drowsiness.
Coccyx injury from fall, with pain radiating up spine and down limbs. Jerking and twitching of muscles. Darting pain in shoulders. Pressure along ulnar side of arm. Cramp in calves. Pain in toes and fingers, especially in tips. Crawling in hand and feet. Lancinating pain in upper and lower limbs. Neuritis, with tingling, burning pain, numbness and flossy skin. Joints feel bruised. Hysterical joints. Tetanus. Traumatic neuralgia and neuritis.
Physostigma Venenosum
This remedy and its active principle, Eserine, form a valuable addition to Materia Medica. Burning and tingling in spine. Hands and feet numb. Sudden jerking of limbs on going to sleep. Tetanic convulsions. Locomotor ataxia. Numbness in paralyzed parts, crampy pains in limbs. Contraction of the pupil and of the ciliary muscles. Spinal irritation, loss of motility, prostration, with very sensitive vertebrae Fibrillary tremors. Rigidity of muscles; paralysis. Depressed motor and reflex activity of the spinal cord, loss of sensibility to pain, muscular weakness, followed by complete paralysis, although muscular contractility is not impaired. Paralysis and tremors, chorea. Meningeal irritation, with rigidity of muscles. Tetanus and trismus. Poliomyelitis anterior.
P. S: This article is only for doctors and students having good knowledge about Homeopathy and allopathy.

For proper consultation and treatment, please visit our clinic.
 Dr. Sayyad Qaisar Ahmed (MD {Ukraine}, DHMS), Abdominal Surgeries, Oncological surgeries, Gastroenterologist, Specialist Homeopathic Medicines.
Dr. Sayyad Qaisar Ahmed (MD {Ukraine}, DHMS), Abdominal Surgeries, Oncological surgeries, Gastroenterologist, Specialist Homeopathic Medicines.
Senior research officer at Dnepropetrovsk state medical academy Ukraine.
Location: Al-Haytham clinic, Umer Farooq Chowk Risalpur Sadder (0923631023, 03119884588), K.P.K, Pakistan.
Find more about Dr Sayed Qaisar Ahmed at:
https://www.youtube.com/Dr Qaisar Ahmed


